مقدمة
العلاج بالموجات الصدمية, medically known as extracorporeal shockwave therapy (ESWT), is a non-invasive treatment widely used in physical medicine, orthopedics, sports rehabilitation, and musculoskeletal care. It delivers controlled acoustic waves to targeted tissues to reduce pain, stimulate healing, and improve functional recovery, particularly in chronic conditions that respond poorly to conventional treatments.
Clinicians increasingly combine shockwave therapy with laser physiotherapy, therapeutic exercise, and manual techniques. To use it safely and effectively, they need a clear understanding of its mechanisms, indications, contraindications, and safety considerations. This article provides an evidence-based overview to help clinicians make informed decisions and deliver safe patient care.
1. What Is Shockwave Therapy
Shockwave therapy uses high-energy acoustic waves generated outside the body and delivers them into biological tissues for therapeutic purposes. Clinicians must understand how shockwaves interact with tissues and the different types of devices available to deliver them to fully appreciate their clinical value.
1.1 Principles of Shockwave Therapy
Shockwave therapy triggers biological responses through mechanical stimulation. The following section explains the physiological mechanisms behind its therapeutic effects.
1.1.1 Mechanism of Action
Shockwave therapy primarily works through mechanotransduction, where mechanical forces convert into biochemical signals within cells. When acoustic shockwaves enter soft tissue, they create rapid pressure fluctuations that stimulate cell membranes, ion channels, and the extracellular matrix. This stimulation triggers the release of growth factors such as vascular endothelial growth factor (VEGF), endothelial nitric oxide synthase (eNOS), and bone morphogenetic proteins (BMPs).
These growth factors enhance angiogenesis, improve local microcirculation, and accelerate tissue regeneration. At the same time, this therapy reduces substance P levels and alters pain signal transmission, which explains its effectiveness in chronic degenerative conditions where poor circulation and tissue metabolism contribute to persistent pain.
1.1.2 Types of Shockwaves
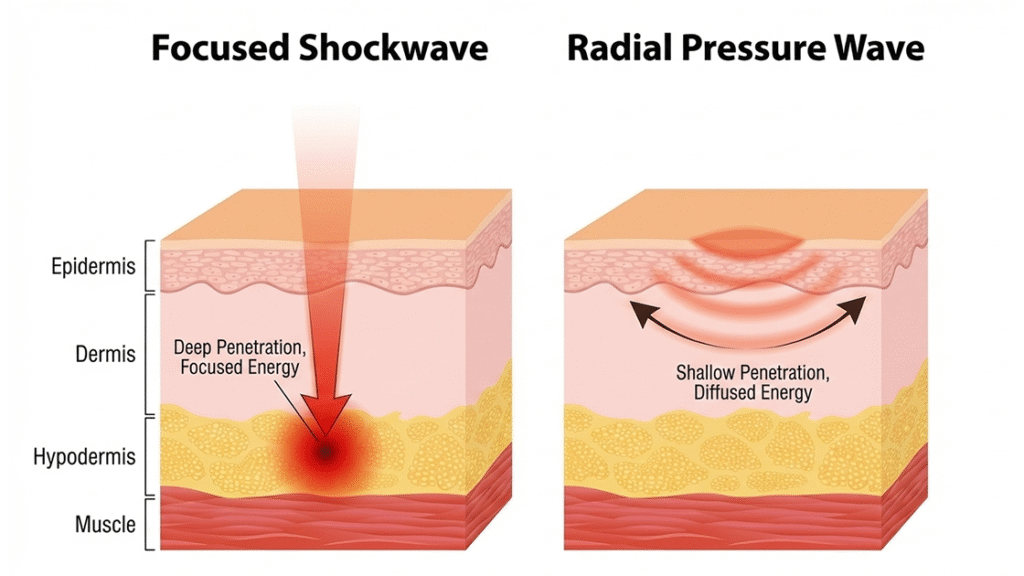
Clinicians deliver shockwave therapy using different technologies with varying energy distribution and penetration depths. Focused shockwaves concentrate energy at a specific deep tissue point, making them ideal for conditions like calcific tendinopathy or delayed bone healing. Radial pressure waves spread energy across a broader, shallower area and are often used for myofascial pain, muscle trigger points, and superficial soft tissue disorders.
Understanding these differences allows clinicians to tailor treatment protocols and combine this therapy effectively with complementary modalities, such as laser therapy and manual rehabilitation.
2. Clinical Indications
Once clinicians understand the biological principles, they can better select patients for treatment. ESWT provides significant benefits for chronic, treatment-resistant conditions.
2.1 Musculoskeletal Conditions
Musculoskeletal disorders represent the most well-supported indications for shockwave therapy. Chronic tendinopathies—such as plantar fasciitis, Achilles tendinopathy, lateral epicondylitis, and patellar tendinopathy—respond well to ESWT because it stimulates collagen remodeling and helps reverse degenerative tissue changes.
In calcific shoulder tendinitis, focused shockwaves break up calcium deposits and improve resorption by increasing local vascular activity. Sports medicine applications include treating muscle trigger points, insertional pain, and chronic overload injuries. Combining ESWT with laser physiotherapy, corrective exercise, and load management enhances functional recovery and reduces the risk of recurrence.
2.2 Urologic and Other Indications
Shockwave therapy also has applications beyond orthopedics. Low-intensity ESWT (Li-ESWT) has shown promise in treating erectile dysfunction by improving endothelial function and penile microcirculation, sometimes restoring spontaneous erectile capacity in selected patients.
Clinicians also explore ESWT for chronic pelvic pain, wound healing, and dermatological concerns like scar remodeling and cellulite. These emerging uses highlight the therapy’s regenerative potential across medical specialties.
3. Contraindications
Despite its benefits, clinicians cannot use shockwave therapy for every patient. Recognizing contraindications ensures safety and ethical practice.
3.1 Absolute Contraindications
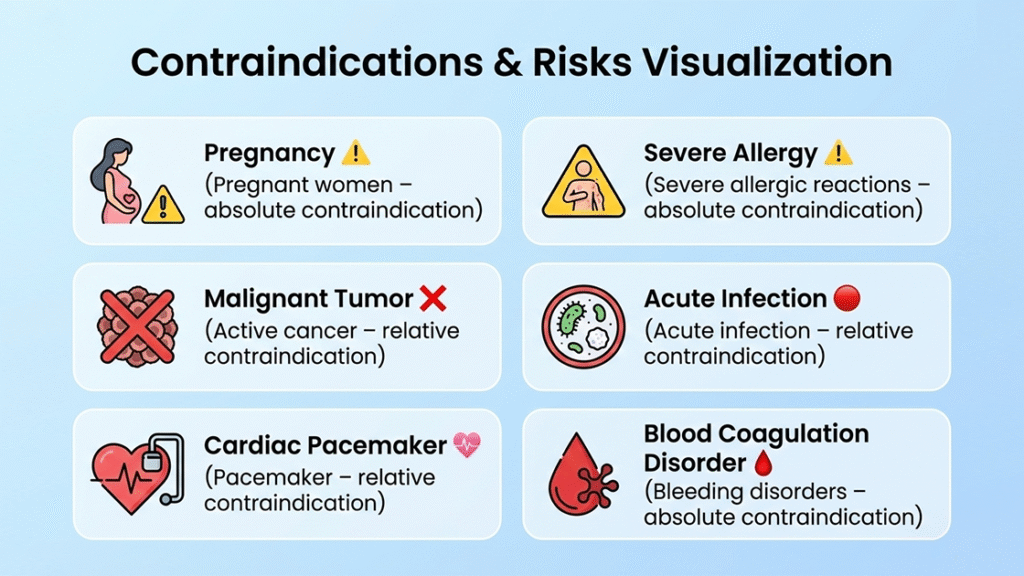
3.1.1 Pregnancy
Clinicians should avoid using shockwave therapy during pregnancy, especially over the abdomen, pelvis, or lumbar spine. The therapy’s mechanical energy may affect fetal development. Although research has not confirmed direct teratogenic effects, clinical guidelines recommend avoiding ESWT in pregnant patients as a precaution.
3.1.2 Malignant Tumor in the Treatment Area
Clinicians should avoid applying shockwave therapy over malignant tissue because it promotes angiogenesis and increases cellular metabolism, which may theoretically accelerate tumor growth or metastasis. They should not use ESWT in areas with known or suspected malignancy.
3.1.3 Severe Coagulation Disorders
Patients with severe coagulation disorders or on high-dose anticoagulants face a higher risk of hematoma or internal bleeding during treatment. The therapy’s mechanical forces can damage fragile blood vessels, so clinicians should avoid ESWT in these patients without specialist clearance.
3.1.4 Electronic Implants (Pacemaker or Defibrillator)
Clinicians should avoid using this therapy near implanted electronic devices. Even though modern devices have better shielding, the therapy can still interfere with their function, especially near the chest area.
3.1.5 Lung Tissue and Air-Filled Areas
Clinicians should not apply shockwaves over lung tissue or other air-filled structures. Sudden acoustic changes at air–tissue interfaces may damage tissue.
3.2 Relative Contraindications
3.2.1 Open Growth Plates in Children
Open epiphyseal growth plates in children are sensitive to mechanical stress. Because evidence is limited, clinicians generally avoid applying shockwave therapy over these areas to protect normal bone development.
3.2.2 Acute Infection or Skin Lesions
Clinicians should postpone treatment if the patient has acute infections, open wounds, or significant skin irritation. Applying mechanical energy under these conditions may worsen inflammation or delay healing.
3.2.3 Recent Corticosteroid Injection
Following corticosteroid injections, tendons and connective tissue may be temporarily weak. Applying shockwave therapy too soon could damage tissues, so clinicians usually wait several weeks before starting ESWT.
4. Risks and Possible Adverse Effects
Discussing risks allows patients to make informed decisions and ensures transparency in clinical practice.
4.1 Common Reactions
Most patients experience only mild, temporary reactions, including localized pain, redness, swelling, or minor bruising at the treatment site. These effects usually resolve within 24–72 hours and indicate a normal physiological response.
4.2 Rare or Serious Complications
Severe complications are uncommon when trained clinicians administer therapy. However, using excessive energy or improper technique can irritate nerves, prolong pain, or damage tissue. Clinicians minimize risk by following evidence-based protocols and carefully selecting patients.
FAQ
What is shockwave therapy used for?
Shockwave therapy is primarily used to treat chronic musculoskeletal pain, tendinopathies, and soft tissue disorders that have not responded to conventional conservative care.
Is shockwave therapy painful?
Some discomfort may be experienced during treatment, but intensity can be adjusted. Most patients tolerate the procedure well.
How does shockwave therapy compare with laser therapy?
Shockwave therapy delivers mechanical energy to stimulate tissue regeneration, while laser therapy uses photobiomodulation to enhance cellular metabolism. They are often combined for synergistic effects.
How many sessions are required?
Typical protocols involve three to six sessions, depending on the condition and patient response.
Who should avoid shockwave therapy?
Pregnant individuals, patients with malignancies in the treatment area, severe coagulation disorders, or implanted electronic devices should avoid ESWT.
الخاتمة
Shockwave therapy is a well-established, evidence-based modality in modern rehabilitation and regenerative medicine. Its ability to promote tissue healing, reduce pain, and improve function makes it a valuable alternative to invasive interventions. Safe and effective use depends on appropriate patient selection, awareness of contraindications, and integration with complementary treatments such as laser physiotherapy and therapeutic exercise.
When applied within clinical guidelines by qualified professionals, shockwave therapy offers a reliable, non-surgical option for managing a wide range of chronic conditions.
المراجع
Shockwave Treatment: A New Wave for Musculoskeletal Care
Mayo Clinic – Physical Medicine and Rehabilitation
Indications and Contraindications for Medical Shockwave Treatment
International Society for Medical Shockwave Treatment (ISMST)
https://shockwavetherapy.org/indications/
Shockwave Therapy Contraindications and Safety Guidelines
https://shockwave-therapy.co.uk/contraindications
Extracorporeal Shock Wave Therapy: A Comprehensive Overview
Physiotherapist India
https://physiotherapistindia.com/shockwave-therapy-a-comprehensive-overview
