Introduction: Rethinking Bone Health
As our understanding of bone physiology evolves, innovative therapeutic approaches are emerging to address one of medicine’s most pressing challenges. The intersection of mechanical medicine and bone biology has opened new pathways for treating skeletal disorders, particularly through non-invasive technologies that harness the body’s natural healing mechanisms.
The Growing Burden of Osteoporosis Worldwide
Osteoporosis affects over 200 million people globally, with approximately 10.3 million Americans living with this debilitating condition. The World Health Organization identifies osteoporosis as a major public health concern, particularly among postmenopausal women and aging populations. The economic burden exceeds $20 billion annually in the United States alone, encompassing direct medical costs, rehabilitation expenses, and lost productivity. Healthcare systems worldwide struggle with the cascading effects of osteoporotic fractures, which often lead to prolonged hospitalization, surgical interventions, and long-term care requirements.
Limitations of Traditional Osteoporosis Treatments
Current pharmacological interventions, including bisphosphonates, selective estrogen receptor modulators (SERMs), and parathyroid hormone analogs, present significant challenges. These medications often cause gastrointestinal disturbances, osteonecrosis of the jaw, atypical femoral fractures, and cardiovascular complications. Patient compliance remains problematic due to complex dosing schedules and adverse effects. Additionally, traditional treatments primarily focus on slowing bone resorption rather than actively promoting bone formation, leaving a therapeutic gap in addressing the fundamental pathophysiology of osteoporosis.
Introducing Shockwave Therapy as a Potential Bone Regenerator
Extracorporeal shockwave therapy (ESWT) represents a paradigm shift from pharmaceutical interventions to mechanical stimulation approaches. This non-invasive modality utilizes acoustic waves to trigger mechanotransduction pathways, potentially stimulating osteoblast activity and bone matrix synthesis. Unlike conventional treatments that require systemic administration, shockwave therapy offers targeted, localized intervention with minimal systemic exposure. The therapy’s ability to enhance cellular metabolism, promote angiogenesis, and stimulate regenerative processes positions it as a promising adjunct or alternative to traditional osteoporosis management strategies.
What Is Osteoporosis?
Understanding the pathophysiology of bone loss provides crucial context for evaluating emerging therapeutic interventions. Osteoporosis represents a complex metabolic disorder characterized by microarchitectural deterioration and compromised bone strength, fundamentally altering the skeletal system’s structural integrity and biomechanical properties.
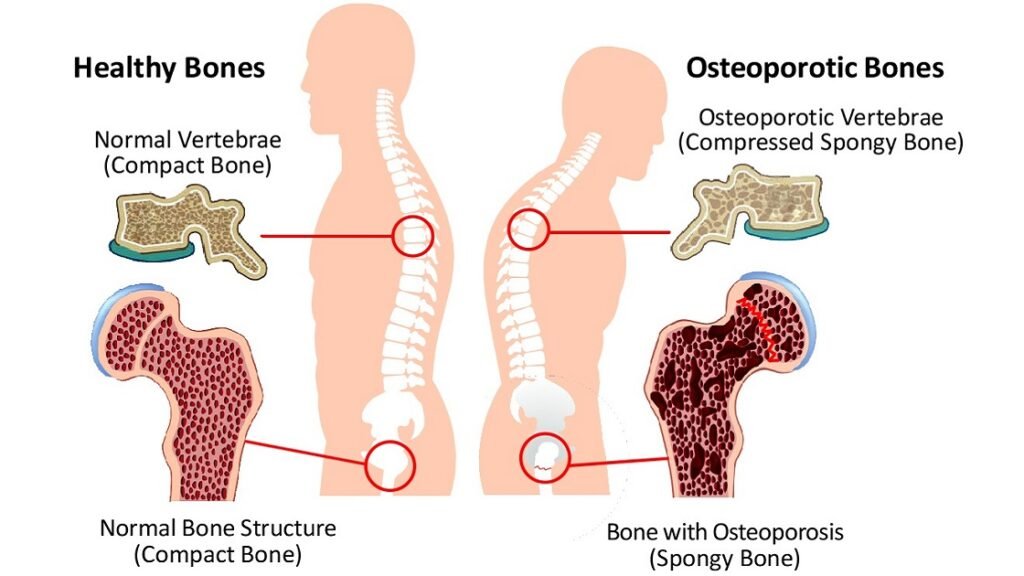
Definition and How It Affects Bone Density
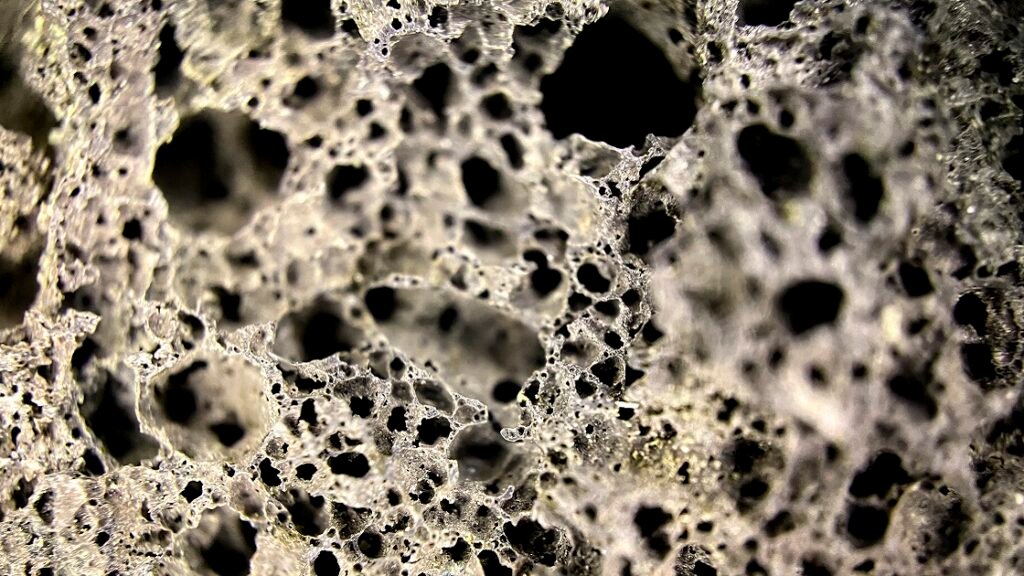
Osteoporosis is clinically defined as a bone mineral density (BMD) T-score of -2.5 or lower, measured by dual-energy X-ray absorptiometry (DEXA). This condition results from an imbalance between bone resorption by osteoclasts and bone formation by osteoblasts, favoring excessive bone breakdown. The trabecular bone architecture becomes compromised, with reduced trabecular thickness, increased trabecular separation, and decreased connectivity. Cortical bone also experiences thinning and increased porosity, collectively reducing the bone’s ability to withstand mechanical stress and increasing fracture susceptibility significantly.
Common Symptoms and Risk Factors
Osteoporosis often remains asymptomatic until fractures occur, earning its designation as a “silent disease.” Early indicators may include height loss, stooped posture (kyphosis), and back pain resulting from vertebral compression fractures. Primary risk factors include advanced age, female gender, estrogen deficiency, genetic predisposition, inadequate calcium and vitamin D intake, sedentary lifestyle, smoking, excessive alcohol consumption, and certain medications including corticosteroids. Secondary causes encompass endocrine disorders, malabsorption syndromes, chronic kidney disease, and inflammatory conditions that affect bone metabolism and mineral homeostasis.
Long-Term Consequences of Untreated Osteoporosis
Progressive bone loss leads to devastating complications, with hip fractures resulting in 20% mortality within one year and 50% permanent disability among survivors. Vertebral compression fractures cause chronic pain, spinal deformity, and reduced quality of life. The cumulative effect of multiple fractures creates a cascade of functional decline, social isolation, and psychological distress. Healthcare utilization increases exponentially, with repeated hospitalizations, surgical procedures, and long-term care placement. The financial burden extends beyond direct medical costs to encompass caregiver expenses, home modifications, and productivity losses affecting entire families.
Understanding Shockwave Therapy
The therapeutic application of acoustic waves in medicine has evolved significantly since its introduction for lithotripsy. Modern shockwave therapy represents a sophisticated approach to tissue regeneration, utilizing precisely controlled mechanical energy to stimulate cellular responses and promote healing processes across various medical specialties.
What Is Shockwave Therapy?
Shockwave therapy employs high-energy acoustic pulses delivered to target tissues through specialized applicators. These pressure waves generate mechanical stress within tissues, initiating mechanotransduction cascades that influence cellular behavior and tissue remodeling. The therapy operates on the principle that controlled mechanical stimulation can enhance the body’s natural healing mechanisms. Clinical applications span orthopedics, urology, cardiology, and wound care, demonstrating the versatility of this therapeutic modality. The non-invasive nature of treatment eliminates surgical risks while providing targeted intervention for specific anatomical regions requiring therapeutic intervention.
Types of Shockwaves: Radial vs. Focused
Radial shockwaves generate pressure waves that spread outward from the applicator tip, creating a broader treatment area with moderate energy density. This type penetrates approximately 30-40mm into tissues and proves effective for superficial musculoskeletal conditions. Focused shockwaves concentrate energy at specific depths within tissues, achieving higher energy densities at precise anatomical targets. The focal point can be adjusted from 10-100mm depth, allowing treatment of deeper structures with greater precision. Energy parameters range from 0.1-0.5 mJ/mm² for radial waves and 0.1-1.0 mJ/mm² for focused applications, with treatment protocols varying based on clinical indications.
How Shockwave Therapy Works at a Cellular Level
Shockwaves induce mechanotransduction through integrin activation, triggering intracellular signaling cascades that influence gene expression and protein synthesis. Mechanotransduction converts mechanical stimuli (pulses of acoustic waves) into a positive cellular healing response. The therapy stimulates nitric oxide production, enhances calcium signaling, and activates growth factors including bone morphogenetic proteins (BMPs) and transforming growth factor-beta (TGF-β). Cellular membrane permeabilization increases nutrient uptake and waste elimination. Angiogenesis is promoted through vascular endothelial growth factor (VEGF) upregulation, improving tissue perfusion and oxygen delivery to support regenerative processes.
Established Uses in Orthopedics and Physical Medicine
Shockwave therapy has gained widespread acceptance for treating plantar fasciitis, lateral epicondylitis, calcific tendinopathy, and non-union fractures. These advantageous properties with a clearly positive cost-benefit ratio make shockwave therapy a first line treatment in delayed and non-union fractures. The therapy demonstrates efficacy in promoting bone healing, reducing chronic pain, and improving functional outcomes. Clinical protocols typically involve 3-5 treatment sessions administered weekly, with energy parameters adjusted based on tissue depth and pathology severity. Success rates range from 60-90% across various musculoskeletal conditions, with minimal adverse effects and high patient satisfaction scores reported in multiple clinical studies.
The Science: Can Shockwave Therapy Treat Osteoporosis?
The scientific foundation for shockwave therapy in osteoporosis treatment builds upon fundamental principles of bone mechanobiology. Research demonstrates that mechanical stimulation can influence bone remodeling processes, offering insights into how acoustic waves might address the pathophysiological mechanisms underlying osteoporotic bone loss.
Mechanical Stress and Bone Remodeling (Mechanotransduction)
Bone tissue responds to mechanical loading through sophisticated mechanotransduction pathways involving osteocytes, osteoblasts, and osteoclasts. Mechanotransduction provides the link between modulation of the extracellular matrix by mechanical load and intracellular activity. Osteocytes detect mechanical deformation through their dendritic processes and canalicular network, releasing signaling molecules that regulate bone formation and resorption. The Wnt/β-catenin pathway plays a crucial role in mechanically-induced bone formation, while sclerostin acts as a negative regulator. Primary cilia on bone cells serve as mechanosensors, detecting fluid flow and transmitting mechanical signals that influence osteoblast differentiation and bone matrix production.
Activation of Osteoblasts and Bone Matrix Production
Shockwave therapy stimulates osteoblast proliferation and differentiation through multiple molecular pathways. ESW therapy promoted bone formation and prevented bone loss on osteoporosis through TGF-β/SMAD2 pathway and osteoblast differentiation can be more effectively promoted by ESW therapy with low energy flow density. The treatment enhances alkaline phosphatase activity, increases collagen type I synthesis, and promotes mineralization of the bone matrix. Growth factors including BMP-2, BMP-7, and insulin-like growth factor-1 (IGF-1) are upregulated following shockwave application. These molecular changes translate into increased bone formation rates and improved trabecular architecture in experimental models of osteoporosis.
Preclinical Evidence: What Animal Models Show
Animal studies provide compelling evidence for shockwave therapy’s bone-forming potential. OP causes a decrease in bone mineral density (BMD), deterioration of bone quality, and micro-architectural fractures of the bone, and research shows that shockwave treatment can address these issues. Ovariectomized rat models demonstrate increased bone mineral density, improved trabecular microarchitecture, and enhanced biomechanical properties following shockwave therapy. Histomorphometric analysis reveals increased osteoblast surface area, bone formation rates, and mineral apposition rates. The therapy also reduces osteoclast activity through NF-κB pathway inhibition. Treatment protocols typically involve low-energy applications (0.1-0.3 mJ/mm²) administered 2-3 times weekly for 4-8 weeks, showing optimal bone formation responses.
Clinical Findings: Delayed Union, Non-Union, and Fragility Fractures
Human clinical studies demonstrate shockwave therapy’s efficacy in promoting bone healing across various scenarios. This study showed that ESWT could efficiently improve the local BMD; relatively, the high dosage was effective. Delayed union and non-union fractures show healing rates of 70-90% following shockwave treatment, often avoiding the need for surgical intervention. Fragility fractures, particularly in osteoporotic patients, demonstrate accelerated healing and reduced time to full weight-bearing. However, a single treatment with unfocused shockwave therapy in unselected patients had any effect in terms of bone mineral density (BMD) or bone mineral content (BMC), suggesting that treatment protocols require optimization for osteoporosis management.
Benefits of Shockwave Therapy for Osteoporosis Patients
The potential advantages of incorporating shockwave therapy into osteoporosis management extend beyond direct bone effects. This therapeutic approach offers a multifaceted intervention that addresses various aspects of bone health while minimizing the complications associated with traditional pharmacological treatments.
Pain Relief Without Drugs or Surgery
Shockwave therapy provides significant analgesic effects through multiple mechanisms, including neuronal hyperstimulation, substance P depletion, and endorphin release. This pain reduction occurs without the gastrointestinal, renal, or cardiovascular risks associated with long-term nonsteroidal anti-inflammatory drug (NSAID) use. Patients with osteoporotic vertebral compression fractures experience substantial pain relief, often within 24-48 hours following treatment. The analgesic effects persist for several months, reducing reliance on opioid medications and their associated dependency risks. This drug-free approach proves particularly valuable for elderly patients with multiple comorbidities and complex medication regimens.
Potential to Improve Bone Strength and Architecture
Beyond pain management, shockwave therapy may directly enhance bone quality through stimulation of bone formation processes. The treatment promotes cortical bone thickening, improves trabecular connectivity, and increases bone mineral density at targeted sites. Biomechanical testing demonstrates improved bone strength and stiffness following shockwave therapy. The therapy’s ability to stimulate osteoblast activity while inhibiting excessive osteoclast function creates a favorable environment for bone formation. These structural improvements translate into reduced fracture risk and enhanced mechanical competence of the skeletal system, addressing the fundamental pathophysiology of osteoporosis.
Supporting Balance, Stability, and Fracture Prevention
Shockwave therapy’s effects extend to surrounding soft tissues, potentially improving muscle strength, proprioception, and balance control. Enhanced neuromuscular function reduces fall risk, which represents a critical component of fracture prevention in osteoporotic patients. The therapy’s analgesic effects allow patients to engage more actively in weight-bearing exercise and physical therapy programs. Improved mobility and reduced fear of movement contribute to better overall functional capacity. The combination of direct bone effects and improved neuromuscular control creates a comprehensive approach to fracture prevention that addresses both bone fragility and fall risk factors.
Enhancing the Effects of Diet, Exercise, and Medication
Shockwave therapy may synergistically enhance other osteoporosis interventions by improving tissue responsiveness and blood flow. Increased vascularization enhances nutrient delivery and medication distribution to bone tissue. The therapy’s effects on bone metabolism may amplify the benefits of calcium and vitamin D supplementation. Improved pain control and mobility facilitate adherence to exercise programs, maximizing the mechanical loading benefits for bone health. When combined with pharmacological treatments, shockwave therapy may reduce required medication dosages while maintaining therapeutic efficacy. This integrative approach addresses osteoporosis through multiple pathways, potentially improving treatment outcomes while minimizing individual intervention risks.
Who Might Benefit Most?
Identifying appropriate candidates for shockwave therapy requires careful consideration of individual patient factors, disease severity, and treatment goals. Certain populations may derive greater benefit from this intervention based on their specific clinical characteristics and risk profiles.
Older Adults with Fragility Fractures or Fall Risk
Elderly patients experiencing osteoporotic fractures represent an ideal population for shockwave therapy intervention. These individuals often have compromised healing capacity, multiple comorbidities, and increased surgical risks that make traditional interventions challenging. The non-invasive nature of shockwave therapy eliminates anesthetic risks while promoting bone healing. Patients with recurrent fragility fractures may benefit from targeted treatment to high-risk anatomical sites. The therapy’s ability to improve pain control and functional mobility addresses immediate quality-of-life concerns while potentially reducing future fracture risk through enhanced bone strength.
Postmenopausal Women with Early Bone Loss
Women in the early postmenopausal period experiencing rapid bone loss may benefit from shockwave therapy as a preventive intervention. This population often experiences accelerated bone turnover due to estrogen deficiency, making them candidates for interventions that promote bone formation. The therapy’s anabolic effects on bone tissue may help counteract the catabolic environment created by hormonal changes. Early intervention with shockwave therapy might delay or prevent progression to established osteoporosis, potentially reducing long-term fracture risk. This approach proves particularly valuable for women who cannot tolerate hormone replacement therapy or prefer non-pharmacological interventions.
Individuals Who Cannot Tolerate Medications
Patients experiencing adverse effects from osteoporosis medications represent another key population for shockwave therapy consideration. Gastrointestinal intolerance to bisphosphonates, contraindications to hormone therapy, or concerns about long-term medication effects may lead patients to seek alternative treatments. The therapy’s minimal side effect profile makes it suitable for patients with multiple drug allergies or interactions. Individuals with kidney disease, who cannot safely use certain osteoporosis medications, may benefit from mechanical intervention approaches. This population often requires personalized treatment strategies that balance efficacy with safety considerations.
Patients with Site-Specific Bone Density Loss
Localized bone loss patterns, such as those occurring around joint replacements or in specific anatomical regions, may be particularly responsive to targeted shockwave therapy. Patients with uneven bone density distribution could benefit from focused treatment of high-risk areas. Regional bone loss following immobilization, stroke, or neurological conditions represents another potential indication. The therapy’s ability to provide targeted intervention without systemic exposure makes it ideal for addressing focal bone loss patterns. Site-specific treatment allows for personalized approaches based on individual bone density patterns and fracture risk assessment.
What to Expect from a Session
Understanding the practical aspects of shockwave therapy helps patients prepare for treatment and develop realistic expectations regarding the therapeutic process. The treatment experience varies based on specific protocols, equipment types, and individual patient factors.

How a Typical Shockwave Therapy Session Works
Treatment sessions typically last 15-30 minutes and begin with patient positioning to optimize access to target areas. The skin is cleaned and ultrasound gel is applied to ensure proper acoustic coupling between the applicator and tissue. The healthcare provider identifies anatomical landmarks and marks treatment areas based on imaging studies or clinical examination findings. Shockwave parameters including energy level, frequency, and pulse number are adjusted according to established protocols. The applicator is moved systematically across treatment areas, delivering controlled acoustic pulses. Patients may feel pressure or mild discomfort during treatment, but anesthesia is rarely required.
Is It Painful? Side Effects and Safety Considerations
Most patients experience minimal discomfort during shockwave therapy, describing sensations as tolerable pressure or mild stinging. Pain levels typically remain below 4/10 on numerical rating scales, and discomfort subsides immediately following treatment completion. Common side effects include temporary skin redness, mild swelling, and occasional bruising at treatment sites. These effects resolve within 24-48 hours without intervention. Contraindications include pregnancy, pacemaker presence, bleeding disorders, active infections, and malignancy at treatment sites. Serious adverse events are rare, with infection rates below 0.1% in reported studies. Pre-treatment assessment ensures patient safety and identifies potential complications.
Frequency and Duration of Treatment Plans
Standard protocols typically involve 3-6 treatment sessions administered at weekly intervals, though specific regimens vary based on clinical indications and patient response. Each session delivers 2000-4000 shock pulses at energy densities ranging from 0.1-0.5 mJ/mm². Treatment frequency may be adjusted based on tissue tolerance and healing response. Some patients may require maintenance treatments every 3-6 months to sustain therapeutic benefits. Response assessment occurs 4-6 weeks following treatment completion using imaging studies, pain scales, and functional measures. Protocols may be modified based on individual response patterns and clinical outcomes.
What the Research Says
The scientific evidence supporting shockwave therapy for osteoporosis continues to evolve, with studies examining various aspects of treatment efficacy, safety, and optimal protocols. Current research provides insights into both the potential benefits and limitations of this therapeutic approach.
Key Studies Supporting Shockwave Therapy for Bone Healing
Multiple clinical trials demonstrate shockwave therapy’s efficacy in promoting bone healing across various scenarios. Studies of delayed union fractures report healing rates of 70-85% following shockwave treatment, with most patients achieving union within 3-6 months. Research in osteoporotic animal models shows significant improvements in bone mineral density, trabecular architecture, and biomechanical properties. Low bone mineral density (BMD) leads to metaphyseal fractures, which are considered of delayed, qualitatively reduced healing resulting in prolonged care phases and increased socioeconomic costs. Extracorporeal shockwave therapy (ESWT) is being investigated as a solution to these challenges. Human studies demonstrate accelerated fracture healing and improved functional outcomes in osteoporotic patients.
Limitations in Current Evidence for Osteoporosis Use
Despite promising results, several limitations characterize the current evidence base for shockwave therapy in osteoporosis. Most studies involve small sample sizes and lack adequate control groups, limiting statistical power and clinical applicability. Extracorporeal shockwave therapy showed a pronounced effect on bone mass in previous animal studies. We showed in this pilot study that a single treatment with unfocused shockwave therapy in unselected patients does not show side effects. Although our research shows mixed results in human applications. Standardized treatment protocols remain undefined, with significant variability in energy levels, frequency, and duration across studies. Long-term follow-up data are limited, preventing assessment of sustained therapeutic benefits and potential complications.
Expert Opinions from Orthopedic and Geriatric Fields
Leading orthopedic specialists acknowledge shockwave therapy’s potential while emphasizing the need for additional research to establish definitive treatment guidelines. Geriatricians express interest in non-pharmacological approaches for osteoporosis management, particularly for patients intolerant of traditional medications. Professional organizations recommend considering shockwave therapy as an adjunct to established treatments rather than a primary intervention. Experts stress the importance of patient selection, appropriate technical training, and realistic outcome expectations. The consensus supports continued research to optimize treatment protocols and identify ideal candidate populations for this emerging therapeutic modality.
Final Thoughts: Is It Worth Trying?
Shockwave therapy offers a promising, non-invasive option for managing osteoporosis, especially in patients who can’t tolerate medications. Its safety, minimal side effects, and potential to stimulate bone regeneration—possibly via the NF-κB signaling pathway—make it an attractive adjunct treatment. However, current evidence remains preliminary. While small studies and animal models show encouraging results, large-scale clinical trials are needed to confirm long-term efficacy and identify ideal candidates. Rather than replacing standard therapies, shockwave treatment should be considered as part of a broader management plan, particularly for those with localized bone loss or healing difficulties. Patients should consult healthcare providers to weigh risks, benefits, and expectations. As research progresses, shockwave therapy may play a more central role in osteoporosis care, but for now, it remains an investigational option worth careful, case-by-case consideration.
FAQs About Shockwave Therapy and Bone Loss
While shockwave therapy doesn’t replace medications, studies suggest it can stimulate osteoblast activity and promote localized bone remodeling, potentially supporting bone density improvement in specific areas.
Yes. When administered by trained professionals, it’s generally safe with minimal side effects—mostly mild, temporary soreness at the treatment site.
It uses high-energy sound waves to trigger mechanotransduction, encouraging cellular repair processes, improved blood flow, and bone formation at targeted sites.
Discomfort is usually mild and temporary. Some patients compare it to a tapping or snapping sensation, which typically fades after the session.
It’s best used alongside standard treatments like calcium, vitamin D, lifestyle changes, or medications—not as a sole therapy.
References and Clinical Sources
- Speed Up Healing: Shockwave Therapy’s Impact on Fracture Repair
- Extracorporeal Shock Wave Therapy Promotes Osteogenic Differentiation in a Rabbit Osteoporosis Model
- Influence of extracorporeal shock wave therapy (ESWT) on bone turnover markers in organisms with normal and low bone mineral density during fracture healing: a randomized clinical trial
- Effect of high-intensity laser therapy versus shockwave therapy on selected outcome measures in osteoporotic long-term hemiparetic patients: a randomized control trial
