Hip bursitis affects millions of people worldwide, causing debilitating pain that can severely impact daily activities and quality of life. While traditional treatments like rest, medication, and injections provide temporary relief for many patients, others continue to struggle with persistent symptoms. This has led to growing interest in alternative therapies, particularly extracorporeal shockwave therapy (ESWT), as a potential game-changer in hip bursitis management. Recent clinical research has shown promising results for shockwave therapy in treating various musculoskeletal conditions, including hip bursitis. With success rates ranging from 56% to 91% in multiple studies, this non-invasive treatment option is gaining recognition among healthcare professionals and patients alike as an effective alternative to more invasive interventions.
Introduction
Understanding the relationship between shockwave therapy and hip bursitis requires examining both the condition itself and how this innovative treatment addresses its underlying mechanisms. Hip bursitis, formally known as greater trochanteric pain syndrome (GTPS), represents one of the most common causes of lateral hip pain in adults, particularly affecting individuals over 40 years of age.
What is Hip Bursitis?
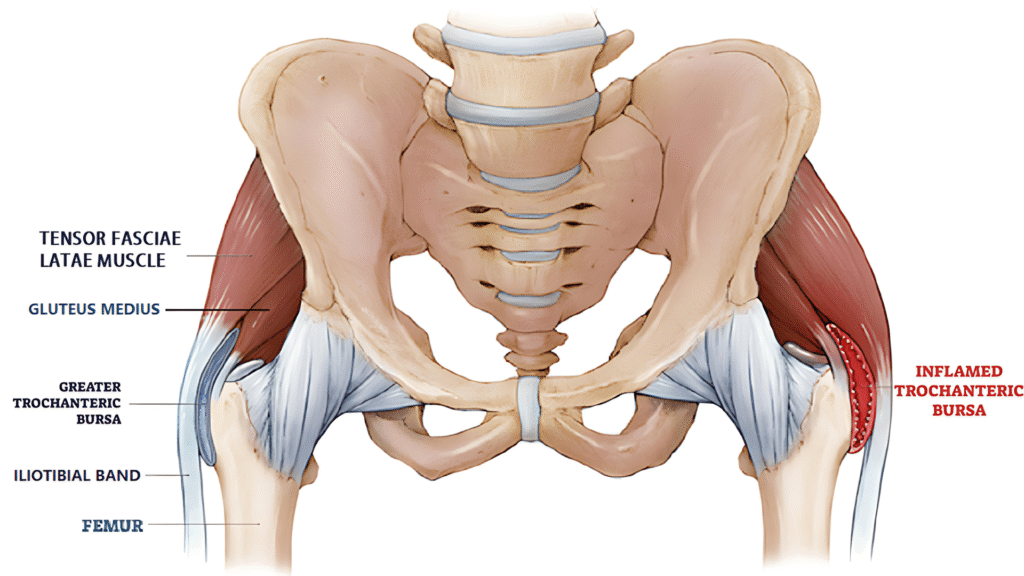
Hip bursitis involves inflammation of the fluid-filled sacs (bursae) that cushion the hip joint, specifically the trochanteric bursa located over the greater trochanter of the femur. These bursae serve as protective cushions between bones, tendons, and muscles, facilitating smooth movement during hip motion. When inflamed, they cause characteristic lateral hip pain that often radiates down the thigh. The condition predominantly affects the greater trochanteric bursa, though the iliopsoas bursa may also be involved. Studies indicate that hip bursitis accounts for approximately 10-25% of all hip-related complaints in orthopedic practices, with a higher prevalence in women than men.
Understanding Shockwave Therapy
Extracorporeal shockwave therapy represents a revolutionary non-invasive treatment modality that utilizes acoustic waves to promote healing in damaged tissues. Originally developed for breaking kidney stones (lithotripsy), this technology has evolved to treat various musculoskeletal conditions over the past 25 years. The therapy involves delivering controlled acoustic pulses to affected tissues through the skin, stimulating biological processes that promote tissue regeneration and pain reduction. Modern shockwave devices can generate either focused or radial waves, each with specific therapeutic applications and energy delivery patterns.
Why Consider Shockwave Therapy for Hip Bursitis?
Traditional hip bursitis treatments often provide only temporary relief, with many patients experiencing symptom recurrence despite multiple interventions. Corticosteroid injections, while effective short-term, may lose efficacy with repeated use and carry potential side effects. Physical therapy, though beneficial, requires significant time commitment and may not address underlying tissue damage. Surgery, reserved for refractory cases, involves inherent risks and extended recovery periods. Shockwave therapy offers a compelling alternative by addressing the root causes of tissue dysfunction while maintaining an excellent safety profile with minimal downtime.
Hip Bursitis: Causes, Symptoms, and Diagnosis
Comprehensive understanding of hip bursitis pathophysiology is essential for appreciating how shockwave therapy provides therapeutic benefits. The condition involves complex interactions between anatomical structures, biomechanical factors, and inflammatory processes that contribute to persistent pain and functional limitation.
Understanding Hip Bursitis Anatomy
The greater trochanteric bursa sits between the greater trochanter of the femur and the overlying iliotibial band and gluteus maximus tendon. This anatomical arrangement makes the bursa susceptible to friction and compression during hip movement, particularly during activities involving repetitive hip abduction or external rotation. The bursa normally contains a small amount of synovial fluid that reduces friction between these structures. When mechanical stress exceeds the bursa’s adaptive capacity, inflammatory mediators are released, leading to increased fluid production, swelling, and pain. Understanding this anatomical relationship helps explain why certain activities exacerbate symptoms and why targeted treatments like shockwave therapy can be effective.
Hip Bursitis Symptoms and Clinical Presentation
Hip bursitis typically manifests as sharp, burning pain over the lateral aspect of the hip, often described as deep and aching. Pain frequently worsens with activities such as climbing stairs, lying on the affected side, or prolonged walking. Many patients report difficulty sleeping due to positional pain, particularly when lying on the affected hip. The pain may radiate down the lateral thigh, sometimes reaching the knee, and can be accompanied by tenderness over the greater trochanter. Morning stiffness and pain with initial movement after prolonged sitting are common complaints. These symptoms can significantly impact functional activities, leading to compensatory movement patterns that may contribute to secondary problems.
Differential Diagnosis
Accurate diagnosis of hip bursitis requires differentiation from other common causes of lateral hip pain, including hip osteoarthritis, lumbar radiculopathy, and gluteal tendinopathy. Hip osteoarthritis typically presents with groin pain and limited range of motion, while lumbar spine pathology may cause radiating pain with neurological symptoms. Gluteal tendinopathy, particularly involving the gluteus medius and minimus tendons, can coexist with bursitis and may require concurrent treatment. Diagnostic imaging, including ultrasound or MRI, can help visualize bursal inflammation and rule out other pathologies. Clinical examination findings, including point tenderness over the greater trochanter and positive Trendelenburg sign, support the diagnosis when combined with appropriate imaging studies.
Traditional Hip Bursitis Treatment Options
Activity Modification
Physical Therapy
Anti-Inflammatory Medications
Corticosteroid Injections
Limitations of Conservative Treatments
Surgical Options
Shockwave Therapy: Mechanism and Applications
The therapeutic effects of shockwave therapy stem from complex biological mechanisms that address both the symptoms and underlying pathophysiology of hip bursitis. Understanding these mechanisms provides insight into why this treatment has shown such promising results in clinical practice.
What Is Shockwave Therapy?
Shockwave therapy utilizes acoustic waves generated by specialized devices to deliver controlled energy to targeted tissues. These high-energy acoustic pulses create pressure variations that propagate through tissues, triggering biological responses at the cellular level. The therapy can be delivered using either focused shockwaves, which concentrate energy at specific depths, or radial shockwaves, which disperse energy more broadly near the treatment surface. Treatment parameters, including energy density, pulse frequency, and session duration, are customized based on the specific condition and patient factors. The non-invasive nature of the treatment allows for outpatient administration without anesthesia, making it an attractive option for many patients.
How Does Shockwave Therapy Work?
The therapeutic mechanisms of shockwave therapy involve multiple biological pathways that promote tissue healing and pain reduction. Acoustic waves create mechanical stress that stimulates cellular metabolism, increases growth factor expression, and enhances blood flow to treated tissues. This process, known as mechanotransduction, triggers the release of angiogenic factors that promote new blood vessel formation (neovascularization). Additionally, shockwaves can disrupt pain signal transmission by affecting nerve endings and may help break down calcifications or scar tissue that contribute to dysfunction. The treatment also stimulates the production of collagen and other extracellular matrix components essential for tissue repair, while reducing inflammatory mediators that perpetuate the pain cycle.
Common Musculoskeletal Conditions Treated
Shockwave therapy has demonstrated efficacy across a wide range of musculoskeletal disorders. Its versatility stems from its ability to stimulate healing, reduce inflammation, and relieve pain. Below are some of the most commonly treated conditions:
Plantar Fasciitis
Tennis Elbow (Lateral Epicondylitis)
Calcific Shoulder Tendinitis
Achilles Tendinopathy
Patellar Tendinopathy (Jumper’s Knee)
Myofascial Pain Syndrome
Scientific Evidence: Shockwave Therapy for Hip Bursitis
The evidence base for shockwave therapy in hip bursitis treatment has grown substantially in recent years, with multiple high-quality studies demonstrating its effectiveness. This research provides valuable insights into treatment outcomes, optimal protocols, and patient selection criteria.
Clinical Studies Overview
Recent systematic reviews and meta-analyses have examined the effectiveness of shockwave therapy for greater trochanteric pain syndrome, providing comprehensive evidence for its therapeutic benefits. A 2024 systematic review and meta-analysis published in Musculoskeletal Care found that shockwave therapy should be considered a viable treatment option for GTPS due to its relatively low incidence of side effects and demonstrated effectiveness. Multiple randomized controlled trials have compared shockwave therapy to traditional treatments, including corticosteroid injections and physical therapy. These studies consistently show significant improvements in pain scores and functional outcomes, with effects often sustained at long-term follow-up. The quality of evidence has improved over time, with more recent studies employing rigorous methodologies and larger sample sizes.
Key Research Findings
The clinical evidence for shockwave therapy in hip bursitis treatment demonstrates consistent benefits across multiple outcome measures, with particular strength in pain reduction and functional improvement domains.
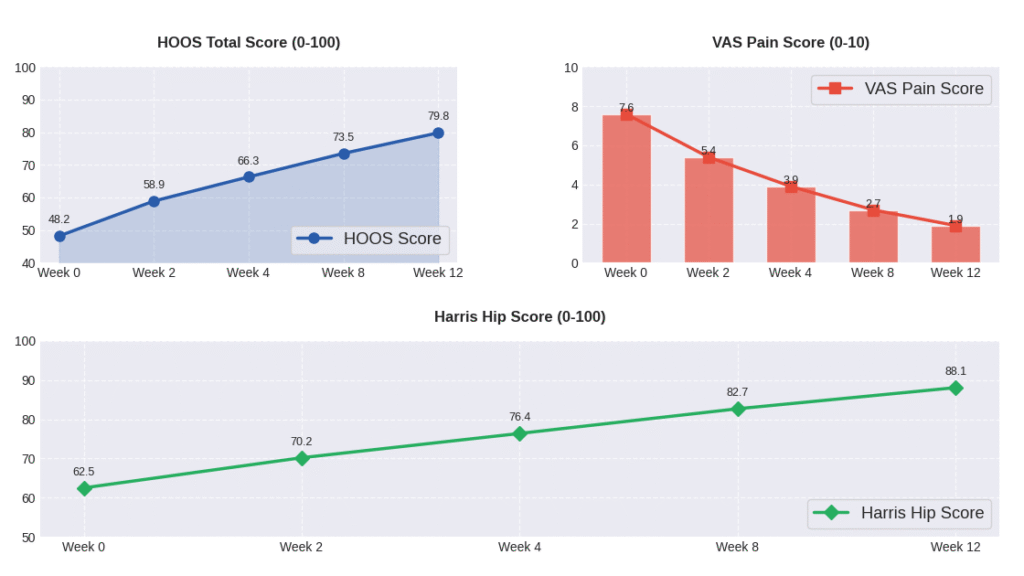
Pain Reduction Outcomes
Clinical studies consistently demonstrate significant pain reduction following shockwave therapy for hip bursitis, with most patients experiencing meaningful improvement within 3-6 weeks of treatment initiation. Visual analog scale (VAS) scores typically decrease by 50-70% from baseline, with many patients achieving clinically significant pain relief defined as a reduction of at least 2 points on a 10-point scale. The pain relief appears to be sustained over time, with follow-up studies showing maintained benefits at 6 and 12 months post-treatment. Importantly, the pain reduction often begins during the treatment course itself, with cumulative effects observed as patients progress through multiple sessions.
Functional Improvement Results
Functional outcomes following shockwave therapy show substantial improvements in activities of daily living and quality of life measures. Hip disability and osteoarthritis outcome score (HOOS) improvements range from 30-60% across multiple studies, with particular benefits noted in pain, symptoms, and activities of daily living subscales. Patients report improved ability to sleep on the affected side, climb stairs, and engage in recreational activities. Return-to-sport rates are particularly impressive among athletic populations, with many patients resuming previous activity levels within 8-12 weeks of treatment completion. These functional improvements often correlate with objective measures of hip strength and range of motion.
Comparative Effectiveness Studies
Direct comparisons between shockwave therapy and traditional treatments reveal favorable outcomes for the acoustic wave approach. Studies comparing shockwave therapy to corticosteroid injections show similar short-term pain relief, but superior long-term outcomes for shockwave treatment. When compared to physical therapy alone, shockwave therapy demonstrates faster onset of pain relief and superior outcomes at 3-month follow-up. Combination therapy approaches, incorporating both shockwave treatment and structured exercise programs, show additive benefits with the highest success rates reported in the literature. These comparative studies provide valuable guidance for treatment selection and sequencing in clinical practice.
Meta-Analysis Results
Meta-analyses pooling data from multiple studies provide the highest level of evidence for shockwave therapy effectiveness in hip bursitis treatment. Recent meta-analyses demonstrate statistically significant improvements in pain and function compared to control groups, with effect sizes ranging from moderate to large. Pooled success rates, defined as greater than 50% pain reduction, range from 65-80% across studies. The number needed to treat (NNT) for achieving clinically meaningful pain relief is approximately 2-3 patients, indicating high treatment efficiency. Subgroup analyses suggest that treatment response may be influenced by factors such as symptom duration, patient age, and concurrent pathology, though these relationships require further investigation.
Limitations of Current Research
Despite growing evidence supporting shockwave therapy for hip bursitis, several limitations in the current research base warrant consideration. Sample sizes in many studies remain relatively small, limiting the power to detect modest treatment effects or identify predictors of response. Follow-up duration varies significantly across studies, with some providing only short-term outcome data that may not reflect long-term treatment durability. Standardization of treatment protocols remains challenging, with variations in energy density, pulse frequency, and session number across studies making direct comparisons difficult. Additionally, most studies focus on patients with isolated hip bursitis, limiting generalizability to patients with concurrent hip pathology or complex presentations.

Treatment Protocol and Patient Selection
Successful shockwave therapy outcomes depend heavily on appropriate patient selection and standardized treatment protocols. Understanding these factors is crucial for optimizing treatment effectiveness and minimizing potential complications.
Ideal Candidates for Shockwave Therapy
- Patients with a confirmed diagnosis of hip bursitis based on clinical evaluation or imaging
- Individuals who have not responded to conservative treatments after at least 6–8 weeks
- Patients without significant concurrent hip pathology, including advanced osteoarthritis or labral tears
- Adults typically between 30 and 70 years of age, though individualized assessment also matters
- Patients who have realistic expectations and are likely to comply with treatment schedules and post-care recommendations
- Those who cannot receive corticosteroid injections or wish to avoid surgical procedures
- Moderately to highly active individuals with clear functional goals, as they tend to show better clinical outcomes
Shockwave Therapy Treatment Protocol
Standard treatment protocols typically involve 3-5 sessions spaced 1-2 weeks apart, though individual variations may be necessary based on patient response and symptom severity. Each session delivers 1500-2500 shock pulses at energy densities ranging from 0.1-0.4 mJ/mm², with precise parameters determined by device specifications and clinical assessment. Treatment duration per session ranges from 15-20 minutes, including setup and positioning time. Patients may experience temporary discomfort during treatment, which is generally well-tolerated without anesthesia. Follow-up assessments are typically scheduled at 2, 6, and 12 weeks post-treatment to monitor progress and determine need for additional sessions. Protocol modifications may be necessary based on individual response patterns and concurrent treatments.
Pre-Treatment Assessment
Comprehensive pre-treatment evaluation ensures appropriate patient selection and establishes baseline measurements for outcome assessment. Clinical history should document symptom duration, previous treatments, functional limitations, and patient goals. Physical examination includes assessment of hip range of motion, strength testing, and identification of tender points. Diagnostic imaging, typically ultrasound or MRI, confirms the diagnosis and rules out concurrent pathologies that might affect treatment planning. Patient education regarding treatment expectations, potential side effects, and post-treatment care is essential for optimal outcomes. Contraindication screening includes assessment for pregnancy, active infection, malignancy, and bleeding disorders. Baseline outcome measures, including pain scales and functional questionnaires, provide objective treatment monitoring tools.
Post-Treatment Care
- Activity Restrictions: Avoid high-impact or strenuous activities for 48 to 72 hours after each shockwave therapy session.
- Gentle Exercises: Perform gentle range-of-motion exercises to maintain joint mobility and promote healing.
- Ice Application: Apply ice packs for 10 to 15 minutes several times a day to reduce temporary discomfort or inflammation.
- Pain Management: Use pain medications as needed, but avoid NSAIDs initially as they may hinder the natural inflammatory process essential for tissue repair.
- Gradual Return to Activity: Slowly resume normal activities over 4 to 6 weeks, guided by symptom improvement and clinical advice.
- Follow-Up Visits: Attend scheduled follow-ups to monitor treatment progress and receive recommendations on activity adjustments.
- Patient Education: Learn to recognize warning signs (e.g., severe pain, swelling, redness) that require prompt medical evaluation.
Effectiveness and Success Rates
Understanding the timeline and magnitude of treatment effects helps patients develop realistic expectations and guides clinical decision-making regarding treatment protocols and follow-up care.
Short-Term Outcomes (0-3 months)
Short-term outcomes following shockwave therapy for hip bursitis are generally favorable, with most patients experiencing some degree of symptom improvement within 2-4 weeks of treatment initiation. Pain reduction typically begins during the treatment course itself, with progressive improvement continuing for several weeks post-treatment. Studies report 60-75% of patients achieving clinically meaningful pain relief (>50% reduction in VAS scores) within 6 weeks of treatment completion. Functional improvements often lag behind pain reduction but become apparent by 8-12 weeks post-treatment. Sleep quality improvements are among the earliest benefits reported, often occurring within the first 2-3 weeks. Patient satisfaction rates during this period range from 70-85%, with most patients reporting they would recommend the treatment to others with similar conditions.
Long-Term Outcomes (6-12 months)
Long-term follow-up studies demonstrate sustained benefits for most patients who respond to initial treatment, with success rates remaining stable or improving over time. Pain relief achieved at 3 months is typically maintained at 6 and 12-month follow-up assessments, with some patients experiencing continued improvement beyond the initial treatment period. Functional outcomes show similar durability, with maintained improvements in activities of daily living and recreational activities. Recurrence rates are relatively low, ranging from 10-20% at one-year follow-up, though these patients often respond well to additional treatment sessions. Return-to-activity rates remain high, with most patients maintaining their desired activity levels throughout the follow-up period. Quality of life measures continue to show benefits, with patients reporting sustained improvements in overall well-being and life satisfaction.
Factors Affecting Treatment Success
- Symptom Duration: Patients treated within 6 months of symptom onset generally achieve better results than those with long-standing symptoms.
- Patient Age: Younger patients (under 50 years) tend to have higher success rates compared to older individuals.
- Body Mass Index (BMI): Normal-weight patients typically respond better to treatment than those with obesity.
- Concurrent Hip Pathologies: Conditions such as hip osteoarthritis or gluteal tendinopathy may reduce the effectiveness of shockwave therapy.
- Treatment Adherence: Compliance with the prescribed therapy sessions and post-treatment activity recommendations is crucial for optimal outcomes.
- Patient Education and Engagement: Educating patients about their condition and the importance of following guidelines enhances treatment success.
Expert Opinions and Clinical Guidelines
Professional perspectives and clinical guidelines provide valuable context for understanding the role of shockwave therapy within the broader landscape of hip bursitis treatment options.
Orthopedic Surgeon Perspectives
Orthopedic surgeons increasingly recognize shockwave therapy as a valuable treatment option for patients with refractory hip bursitis, particularly those seeking alternatives to repeated corticosteroid injections. Many specialists appreciate the treatment’s non-invasive nature and favorable safety profile, making it an attractive option for patients with multiple comorbidities or contraindications to other treatments. Surgeon perspectives emphasize the importance of proper patient selection and realistic expectation setting, noting that while highly effective for many patients, shockwave therapy may not be appropriate for all cases. Integration into practice patterns varies, with some surgeons offering in-office treatment while others refer to specialized centers. The growing body of evidence supporting shockwave therapy has led to increased acceptance among orthopedic specialists, though some remain cautious pending longer-term outcome data.
Physical Medicine and Rehabilitation Views
Physical medicine and rehabilitation specialists tend to view shockwave therapy as an excellent complement to comprehensive rehabilitation programs, particularly when combined with targeted exercise interventions. These specialists emphasize the importance of addressing underlying biomechanical factors that contribute to hip bursitis, viewing shockwave therapy as one component of a multimodal treatment approach. Many appreciate the treatment’s ability to accelerate healing and reduce pain, potentially enhancing patient participation in rehabilitation activities. The non-pharmacological nature of the treatment aligns well with rehabilitation philosophy, avoiding potential complications associated with medications or injections. Integration with traditional physical therapy appears particularly beneficial, with combination approaches showing superior outcomes compared to either treatment alone.
Current Clinical Guidelines
Current clinical guidelines for hip bursitis treatment have begun to incorporate shockwave therapy as a recommended option for patients who fail initial conservative management. Professional organizations, including various orthopedic and sports medicine societies, have developed position statements supporting the use of shockwave therapy for musculoskeletal conditions, though specific guidelines for hip bursitis remain limited. The American Academy of Orthopaedic Surgeons (AAOS) acknowledges extracorporeal shockwave therapy as a treatment option for various tendinopathies, though specific recommendations for hip bursitis await further evidence development. International guidelines show increasing acceptance, with European and Asian medical societies providing more specific recommendations for shockwave therapy in hip pain management. Future guideline updates are expected to provide more detailed recommendations as the evidence base continues to expand.
FAQs
Many patients notice reduced pain within a few sessions, but full benefits often develop gradually over 4 to 8 weeks as healing progresses.
Most people experience mild discomfort during treatment, often described as a tapping sensation. It’s usually well-tolerated and brief, with no anesthesia required.
Typically, 3 to 5 sessions spaced one week apart are recommended, but the exact number depends on individual response and severity.
For many, yes. It offers a non-invasive alternative that promotes natural healing without the risks associated with injections or surgery.
Side effects are generally mild and temporary, such as slight redness or soreness at the treatment site. Serious complications are rare.
People with bleeding disorders, infections, or implanted medical devices like pacemakers should avoid shockwave therapy. Always consult your doctor first.
Conclusion
Shockwave therapy is emerging as a promising non-invasive treatment for hip bursitis, with numerous high-quality studies reporting 65–80% success rates in pain relief and functional improvement. Its ability to target underlying tissue pathology—rather than merely mask symptoms—sets it apart from conventional approaches. With an excellent safety profile and growing clinical support, shockwave therapy is particularly suitable for patients who have not responded to conservative treatments. While not ideal for everyone, appropriately selected patients can expect meaningful and sustained benefits. As research continues to refine protocols and identify optimal candidates, shockwave therapy is likely to become a key tool in hip bursitis management. Patients should consult qualified healthcare professionals to assess whether this treatment suits their individual condition. Its integration into clinical practice reflects a shift toward evidence-based, minimally invasive care that balances effectiveness with safety—offering new hope for lasting relief from hip bursitis.
References
- Unleashing Comfort with Shockwave Therapy for Bursitis
- Shockwave Waves Soothe Aching Bursitis
- Shock Waves and Therapeutic Exercise in Greater Trochanteric Pain Syndrome: A Prospective Randomized Clinical Trial with Cross-Over
- Investigating the Effect of Extracorporeal Shock Wave Therapy on Reducing Chronic Pain in Patients with Pes Anserine Bursitis: A Randomized, Clinical- Controlled Trial
- Is shockwave therapy effective in the management of greater trochanteric pain syndrome? A systematic review and meta-analysis
