Introduction: The IT Band’s Breaking Point
Runners know the frustration when a persistent pain on the outside of the knee derails their training. This pain often originates from the iliotibial band (IT band), a key structure that supports knee stability during movement. Understanding the anatomy and function of the IT band, along with why runners are especially vulnerable to injury, is essential to recognizing and managing this common ailment. In this section, we explore what the IT band is, why it tends to cause problems for runners, and the significant impact chronic pain can have on performance and overall well-being.
What Is the Iliotibial Band?
The iliotibial band is a thick, fibrous connective tissue extending from the iliac crest of the pelvis down the lateral thigh to the tibial tubercle. Unlike muscles, the IT band is a dense fascia that stabilizes the knee during dynamic activities by working synergistically with the tensor fasciae latae and gluteus maximus muscles. It plays a vital role in lateral knee support and load distribution during flexion and extension. However, excessive tension or friction—particularly where the band crosses the lateral femoral epicondyle—can lead to irritation and inflammation, clinically known as iliotibial band syndrome (ITBS). This pathology is especially prevalent among athletes performing repetitive knee movements.
Why Runners Are Prone to IT Band Syndrome
Runners face a heightened risk of developing IT band syndrome due to the repetitive nature of their knee motions. The constant bending and straightening of the knee during running can increase friction between the IT band and the lateral femoral epicondyle. Contributing factors include overtraining, biomechanical imbalances such as hip abductor weakness, improper running form, and inadequate footwear. These elements can cause the IT band to tighten excessively, leading to microtrauma and chronic inflammation. Environmental conditions like running downhill or on uneven surfaces can exacerbate symptoms. Recognizing these risks is critical for prevention and targeted treatment.
The Toll of Chronic Lateral Knee Pain on Performance
Chronic IT band pain does more than cause discomfort—it undermines a runner’s ability to train and compete effectively. Persistent inflammation compromises lateral knee stability and may alter gait mechanics, forcing compensations that can provoke secondary injuries in the hips, ankles, or lower back. Many runners reduce training volume or intensity to manage pain, potentially impeding progress and causing frustration. Over time, untreated ITBS can evolve into degenerative tendinopathy with fibrotic changes, prolonging recovery and limiting athletic longevity. This underlines the importance of timely, evidence-based interventions that address both symptoms and underlying biomechanical causes.
Understanding the Enemy: IT Band Syndrome Demystified
To combat IT band syndrome effectively, it is important to fully understand its clinical presentation, multifactorial causes, and why conventional treatments often fall short. This section breaks down the typical symptoms, pathophysiology, and limitations of standard care, setting the stage for advanced therapeutic options like shockwave therapy.
Common Symptoms of IT Band Syndrome
IT band syndrome usually presents as a sharp, burning, or aching pain localized to the lateral knee region, especially over the lateral femoral epicondyle. Patients often report tenderness on palpation and may experience a snapping or popping sensation during knee flexion and extension. Pain typically worsens with activities involving repetitive knee bending, such as running, cycling, or descending stairs. In some cases, mild swelling or localized inflammation is evident. Symptoms generally improve with rest but tend to recur upon resumption of activity. Early recognition of these hallmark signs allows for prompt diagnosis and management, reducing the risk of progression to chronic tendinopathy.
Causes: Overuse, Biomechanics, and Muscle Imbalances
The pathogenesis of IT band syndrome is multifactorial, stemming primarily from repetitive mechanical overload and biomechanical dysfunction. Overuse through excessive training volume or intensity leads to microtrauma and inflammation at the IT band’s insertion site. Biomechanical factors such as excessive foot pronation, leg length discrepancies, and poor running form increase strain on the IT band. Additionally, weakness or poor activation of hip abductors and core stabilizers disrupts normal gait mechanics, intensifying lateral knee stress. These combined factors exacerbate friction and compressive forces at the lateral femoral epicondyle, perpetuating the inflammatory cycle characteristic of ITBS.
Traditional Treatment Options and Their Shortcomings
Conventional management of IT band syndrome typically includes rest, activity modification, nonsteroidal anti-inflammatory drugs (NSAIDs), physical therapy, stretching, and corticosteroid injections. While these methods aim to reduce pain and inflammation, they often provide only temporary relief without addressing the underlying biomechanical contributors. NSAIDs and corticosteroids carry risks of side effects and may impede long-term tissue healing. Physical therapy can be effective but requires patient adherence and can be slow to resolve symptoms. In many cases, persistent inflammation leads to fibrotic changes in the fascia, limiting recovery and increasing recurrence risk. These limitations highlight the need for more advanced, regenerative therapies such as shockwave therapy.
Enter Shockwave Therapy: The Science of Pain Relief
After understanding the challenges of IT band syndrome and limitations of traditional treatments, many runners seek innovative, evidence-based solutions. Shockwave therapy has emerged as a promising, non-invasive modality specifically designed to target soft tissue injuries like IT band inflammation. This section explains what shockwave therapy is, how it biologically affects the IT band, and the clinical research supporting its use for tendinopathies.
¿Qué es la terapia de ondas de choque?
Shockwave therapy, also known as extracorporeal shockwave therapy (ESWT), is a non-invasive treatment that delivers high-energy acoustic waves to affected tissues. These waves propagate through the skin to penetrate deep into tendons and fascia, stimulating physiological processes that promote healing. Originally developed for kidney stone fragmentation, ESWT has been adapted for musculoskeletal conditions, including tendinopathies and myofascial pain. The mechanical stimulation activates cellular repair mechanisms without surgical intervention, reducing pain and improving function. It is particularly effective for chronic conditions resistant to conventional therapy, offering a scientifically validated alternative for athletes struggling with persistent IT band syndrome.
How It Works on IT Band Inflammation
Understanding the mechanisms by which shockwave therapy alleviates IT band inflammation is essential for appreciating its therapeutic value. The acoustic waves induce a cascade of biological responses that promote tissue regeneration and pain relief. These effects include enhanced blood circulation, mechanical disruption of pathological tissue, and stimulation of cellular repair pathways. Each process addresses key pathological features of IT band syndrome, from reducing inflammation to remodeling scar tissue, thereby restoring normal tissue function.
Estimular el flujo sanguíneo
One of the primary benefits of shockwave therapy is its ability to enhance microcirculation within the targeted tissues. The acoustic waves induce mechanical stress on endothelial cells lining blood vessels, triggering the release of angiogenic factors such as vascular endothelial growth factor (VEGF). This promotes the formation of new capillaries (neovascularization) and improves oxygen and nutrient delivery to the inflamed IT band. Increased blood flow facilitates removal of metabolic waste and inflammatory mediators, accelerating the healing process and reducing pain. Improved vascularization also supports cellular metabolism, essential for tissue repair in chronic tendinopathies.
Breaking Up Scar Tissue
Chronic IT band syndrome often leads to the formation of fibrotic scar tissue and adhesions, which restrict normal tissue elasticity and cause pain. Shockwave therapy exerts mechanical forces that help to disrupt these pathological collagen cross-links. This process, called mechanotransduction, induces microtrauma that stimulates fibroblast activity and collagen remodeling. By breaking down dense scar tissue, the therapy restores tissue flexibility and reduces mechanical irritation at the lateral femoral epicondyle. This remodeling effect improves biomechanical function and reduces the chronic friction that perpetuates IT band inflammation.
Triggering Cellular Regeneration
Beyond physical disruption, shockwave therapy activates molecular pathways involved in tissue regeneration. The mechanical stimulus upregulates growth factors such as transforming growth factor-beta (TGF-β) and nitric oxide synthase (NOS), which modulate inflammation and promote repair. It also stimulates mesenchymal stem cells and fibroblasts to proliferate and synthesize extracellular matrix components necessary for tendon healing. These cellular responses accelerate collagen synthesis and reorganization, facilitating the restoration of normal tendon architecture. The enhanced regenerative capacity helps resolve chronic inflammation and strengthens the IT band, reducing susceptibility to future injury.
Clinical Evidence Supporting Shockwave for Tendinopathies
Numerous clinical trials and meta-analyses validate shockwave therapy as an effective treatment for tendinopathies, including IT band syndrome. Studies demonstrate significant improvements in pain scores, functional outcomes, and return-to-activity timelines compared to placebo or conservative treatments. Shockwave therapy has shown to reduce pro-inflammatory cytokines and improve tendon morphology on imaging. Its safety profile is favorable, with minimal adverse effects reported. For runners, this translates into a scientifically supported option that addresses both symptom relief and underlying pathology. Current guidelines recommend ESWT as part of a multimodal approach for chronic IT band pain resistant to physical therapy and pharmacologic interventions.
The Treatment Process: What Every Runner Should Know
Having explored the science and evidence, the next important aspect is understanding what the actual treatment entails. This section outlines the typical clinical pathway for runners considering shockwave therapy, covering assessment, session frequency, side effects, and practical advice on activity levels during treatment.
Consulta inicial y diagnóstico
The treatment journey begins with a comprehensive clinical evaluation by a sports medicine physician or physical therapist experienced in musculoskeletal disorders. Diagnosis typically involves a detailed patient history, physical examination focusing on pain localization and biomechanical assessment, and imaging studies like ultrasound or MRI to rule out differential diagnoses. Accurate identification of IT band syndrome is critical to customize the shockwave protocol. During the consultation, clinicians discuss treatment goals, contraindications, and expected outcomes. Establishing clear communication helps set realistic expectations and ensures patient compliance throughout the therapy process.
Number of Sessions Needed
Shockwave therapy for IT band syndrome usually requires multiple sessions spaced over several weeks to maximize therapeutic effects. The standard treatment protocol involves 3 to 5 sessions, typically administered once weekly. Each session lasts approximately 15 to 20 minutes, delivering a calibrated number of acoustic pulses at specified energy flux densities. Treatment frequency and duration may be adjusted based on patient response and severity of symptoms. Clinical improvement often becomes noticeable after 2 to 3 sessions, with continued benefits up to several months post-treatment. Adherence to the full course is essential for sustained recovery and prevention of symptom recurrence.
Side Effects and Aftercare Tips
Shockwave therapy is generally well-tolerated, but patients may experience mild, transient side effects. Common reactions include localized redness, swelling, bruising, or discomfort at the treatment site, which typically resolve within 24 to 72 hours. Rarely, more significant pain or skin irritation may occur but usually subsides with conservative care. Aftercare recommendations emphasize rest for 24 to 48 hours post-treatment, avoiding strenuous activities that stress the IT band. Applying ice or anti-inflammatory measures may help manage discomfort. Gradual return to exercise is encouraged under clinical guidance to optimize healing while minimizing reinjury risk.
Can You Run During Treatment?
Many runners wonder if they can maintain training while undergoing shockwave therapy. The answer depends on individual symptom severity and clinician advice. In mild to moderate cases, light running or cross-training may be permitted with close monitoring of pain levels. However, high-intensity or long-distance running is often discouraged during the active treatment phase to prevent aggravation. A graduated rehabilitation program, including strengthening and flexibility exercises, complements shockwave therapy to restore proper biomechanics. Ultimately, pacing activity and prioritizing recovery help ensure treatment efficacy and a safe, faster return to full running performance.

Prevention Is Key: Staying IT Band Pain-Free
While shockwave therapy offers an effective solution for IT band syndrome, preventing recurrence is paramount for long-term running success. Prevention involves targeted strengthening, biomechanical adjustments, and dedicated recovery routines. Understanding how to support the IT band through muscular balance and proper habits ensures sustained relief and improved performance.
Strengthening the Glutes and Core
One of the primary contributors to IT band syndrome is weakness or imbalance in the hip stabilizers, particularly the gluteus medius and maximus muscles. These muscles play a critical role in controlling femoral internal rotation and pelvic stability during the gait cycle. Insufficient gluteal strength increases lateral tension on the IT band, exacerbating friction at the knee. Incorporating focused resistance exercises—such as clamshells, lateral band walks, and hip thrusts—can restore muscular balance. Additionally, core stabilization exercises enhance pelvic control and reduce compensatory movement patterns that overload the IT band. Regular strengthening routines not only protect the IT band but also improve overall running efficiency and injury resilience.
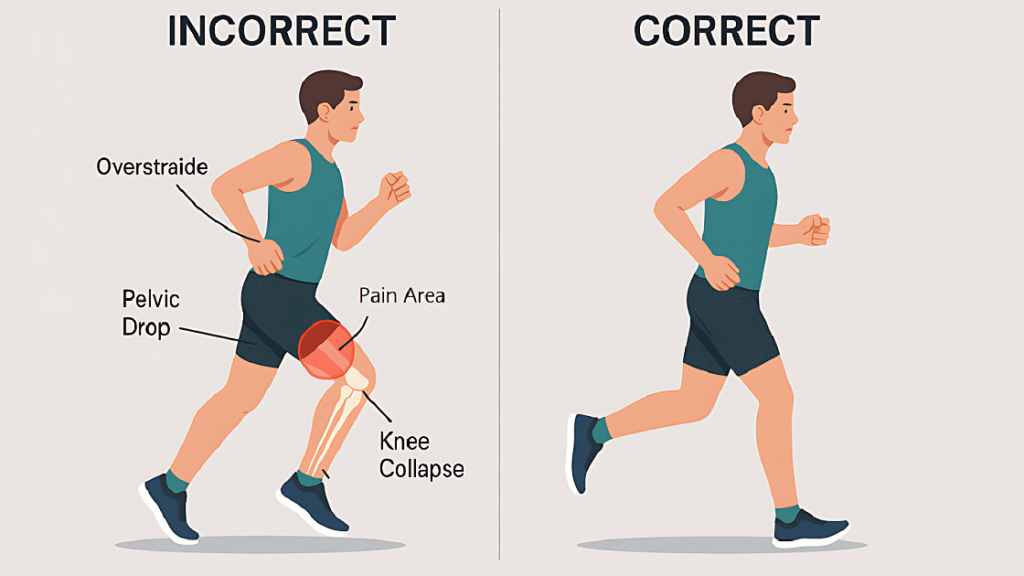
Proper Running Form and Footwear
Biomechanical factors heavily influence IT band stress, making running form and footwear crucial for prevention. Maintaining a midfoot strike, avoiding overstriding, and promoting a slight forward lean optimize kinetic chain alignment and reduce excessive knee adduction moments. Additionally, hip drop or pelvic tilt should be corrected through gait retraining to decrease lateral knee load. Footwear selection is equally important; shoes that provide adequate arch support, shock absorption, and stability tailored to an individual’s foot type can correct abnormal pronation or supination, which indirectly strains the IT band. Periodic gait analysis by a trained professional can help runners identify and modify detrimental movement patterns, reducing the risk of IT band syndrome recurrence.
Importance of Stretching and Recovery Tools
Incorporating regular stretching and recovery modalities is vital for maintaining IT band health and preventing tightness that leads to inflammation. Dynamic warm-ups before runs increase tissue elasticity, while static stretching post-run targets the tensor fasciae latae, quadriceps, hamstrings, and gluteal muscles to relieve tension on the IT band. Foam rolling and myofascial release techniques help break down fascial adhesions and improve tissue mobility, reducing friction and irritation. Additionally, modalities such as cold therapy, compression sleeves, and active recovery sessions promote circulation and decrease inflammatory responses. Consistent recovery protocols complement strengthening and biomechanical corrections, creating a holistic approach to injury prevention.
Conclusion: Get Back to the Finish Line, Faster
IT band syndrome can significantly hinder a runner’s journey, but with targeted interventions like shockwave therapy and a comprehensive prevention plan, recovery and performance restoration are achievable. Terapia de ondas de choque accelerates healing by enhancing blood flow, disrupting scar tissue, and stimulating cellular repair, effectively addressing chronic inflammation and pain. However, long-term success depends on strengthening key muscle groups, optimizing running biomechanics, and committing to regular stretching and recovery strategies. By integrating these evidence-based approaches, runners can break free from IT band pain and confidently return to training and competition. Remember, prevention is the foundation of lasting relief—investing in your body’s mechanics and recovery today means crossing future finish lines stronger and pain-free.
FAQs About Shockwave Therapy for IT Band Pain
It’s safe for most runners but not recommended for those with infections, blood disorders, pregnancy, or cancer near the area. A medical evaluation ensures it’s suitable for each individual.
Light running is usually allowed, but high-impact or intense runs should be avoided to prevent aggravating inflammation. Your clinician will advise based on your progress.
Typically, 3 to 6 sessions spaced weekly or biweekly are needed. Many patients feel improvement after a few treatments, but completing the full course is important.
It not only reduces pain but also promotes tissue repair and strengthens the area, helping lower the risk of future injuries when combined with proper training and prevention.
Some may experience mild soreness, redness, or swelling temporarily. The treatment is generally well tolerated and does not require anesthesia.
