Introduction: Why Old Injuries Still Hurt
The saying “time heals all wounds” doesn’t always apply to sports injuries. For many athletes and active individuals, old injuries become chronic sources of pain that resist traditional treatments. Unlike acute injuries that follow predictable healing timelines, chronic conditions often involve scar tissue buildup, tendon degeneration, and disrupted cellular repair—creating a cycle of inflammation and dysfunction. These unresolved injuries can limit performance, reduce mobility, and negatively impact quality of life. Frustration grows when months or even years of rest, medication, or physical therapy yield little progress. That’s where Extracorporeal Shockwave Therapy (ESWT) enters the picture. This non-invasive treatment uses acoustic waves to reactivate the body’s healing process, break down scar tissue, and reduce pain at its source. ESWT has become a promising option for athletes seeking long-term relief and a return to active living—without surgery or extended downtime.
Understanding Old Sports Injuries
Before exploring how shockwave therapy can address chronic conditions, it’s essential to understand the complex nature of persistent sports injuries and why conventional healing mechanisms sometimes fail to resolve these conditions effectively.
What Qualifies as an Old Sports Injury?
An old sports injury is typically defined as a musculoskeletal condition that has persisted for more than three months beyond the expected healing timeframe, or has become a recurrent problem despite apparent initial resolution. These injuries often involve tendons, ligaments, muscles, and surrounding soft tissues that have undergone pathological changes due to repetitive stress, inadequate healing, or biomechanical dysfunction. Common characteristics include chronic pain, reduced range of motion, functional limitations, and structural abnormalities visible on imaging studies such as ultrasound or MRI. The transition from acute to chronic injury involves complex cellular and molecular changes that distinguish these conditions from fresh traumatic injuries. Chronic injuries often exhibit degenerative tendinopathy, characterized by collagen fiber disorganization, increased ground substance, and neovascularization. These changes create a self-perpetuating cycle where normal healing processes become disrupted, leading to persistent symptoms that resist traditional treatment approaches.
Why Injuries Resurface Years Later
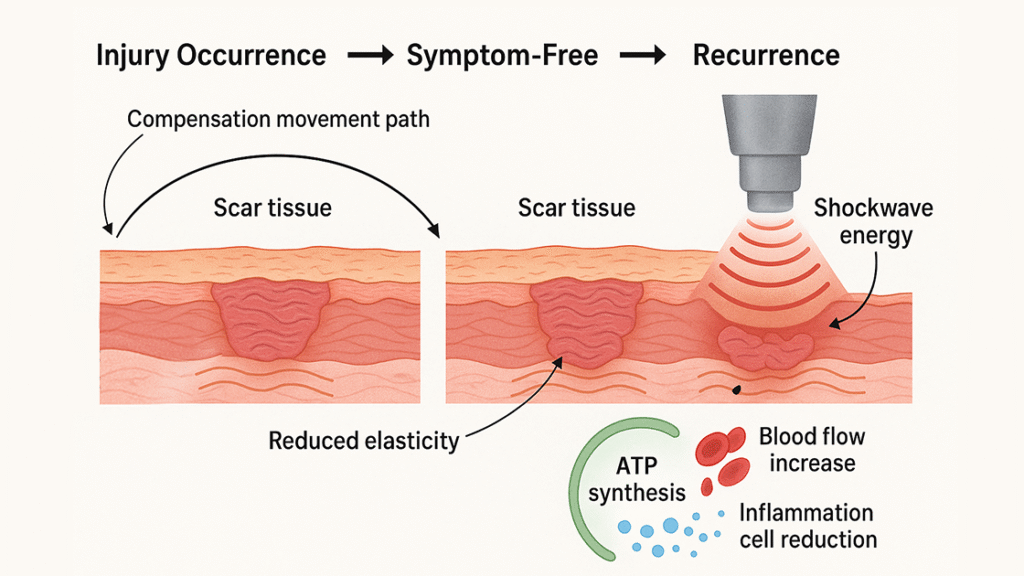
Scar tissue weakness: Healed areas often contain collagen-poor scar tissue that lacks the strength and elasticity of healthy tissue, making them prone to reinjury.
Compensatory movement patterns: Improper mechanics developed during the original injury can persist and strain both the injured and surrounding areas.
Age-related degeneration: Aging slows collagen production and cellular repair, making tissues more susceptible to breakdown over time.
Lifestyle changes: Weight gain, decreased activity, or a return to intense physical activity without adequate preparation can overload vulnerable tissues.
Environmental triggers: Weather changes, occupational demands, or seasonal sport participation can aggravate old injury sites unexpectedly.
Impacto en la calidad de vida
Chronic sports injuries extend far beyond physical discomfort, creating profound impacts on psychological well-being, social relationships, and overall life satisfaction. The persistent nature of these conditions often leads to activity avoidance, decreased fitness levels, and social isolation from sports communities that previously provided identity and fulfillment. Many athletes experience depression, anxiety, and loss of self-esteem when unable to participate in activities that once defined their lifestyle and social connections. The economic burden of chronic injuries includes direct medical costs, lost productivity, and reduced earning potential, particularly for professional athletes whose careers depend on optimal physical performance. Additionally, the ripple effects extend to family members and support systems who must adapt to the limitations and emotional challenges associated with chronic pain conditions. The frustration of failed treatment attempts and the uncertainty about future function create additional psychological stress that can exacerbate pain perception and delay recovery.
¿Qué es la terapia de ondas de choque?
Understanding the scientific foundation of shockwave therapy is crucial for appreciating its potential in treating chronic sports injuries. This innovative treatment modality represents a significant advancement in non-invasive musculoskeletal medicine.
Definition and Mechanism
Extracorporeal shock waves are high-intensity mechanical waves (500–1000 bar) of a microsecond duration with a morphology characterized by a rapid positive phase followed by a negative phase. ESWT works by the emission of acoustic waves (shockwaves) that carry energy and can propagate through tissues. These acoustic waves are generated externally and focused on specific treatment areas without requiring surgical intervention or penetration of the skin barrier. The mechanism involves the conversion of electrical energy into mechanical energy through specialized transducers that create pressure waves capable of penetrating deep into tissues. The Focus shockwave uses a 10-nanosecond burst and allows the provider to send pulses deeper into the body, as much as 13 or 14 centimeters. The Radial shockwave sends pulses in 5 to 10 microseconds and reaches a depth of 3 to 6 centimeters. The therapeutic effects occur through mechanotransduction, where mechanical forces are converted into biochemical signals that stimulate cellular repair processes.
Biological Effects on Tissue
The biological effects of shockwave therapy involve multiple mechanisms that work synergistically to promote tissue healing and pain reduction. Some of the proposed mechanisms of action for ESWT include increased collagen synthesis, cellular proliferation and wound healing, pain reduction, and neovascularization. These effects result from the mechanical stress created by acoustic waves, which triggers various cellular responses including the release of growth factors, activation of stem cells, and stimulation of angiogenesis. The therapeutic process begins with cavitation effects, where rapid pressure changes create microscopic bubbles in tissue fluids that collapse and generate secondary mechanical forces. This cavitation process disrupts pathological tissue formations, breaks down calcifications, and stimulates cellular metabolism. Additionally, the mechanical stress activates mechanosensitive ion channels in cell membranes, leading to increased intracellular calcium levels and activation of various signaling pathways that promote tissue regeneration and pain modulation.
Why Shockwave Therapy Works for Chronic Injuries
The effectiveness of shockwave therapy in treating chronic sports injuries stems from its ability to address the underlying pathophysiological mechanisms that perpetuate these conditions. Understanding these mechanisms helps explain why this treatment succeeds where conventional therapies often fail.
Rebooting the Healing Cycle
Chronic injuries often become trapped in a state of incomplete healing, where normal regenerative processes stall due to poor vascularization, cellular dysfunction, or persistent inflammation. Shockwave therapy essentially “reboots” the healing cycle by creating controlled microtrauma that stimulates the body’s natural repair mechanisms. This process activates dormant healing pathways and promotes the recruitment of healing cells to the injured area. The controlled tissue disruption caused by shockwaves triggers an acute inflammatory response that, unlike chronic inflammation, is beneficial for healing. This acute response promotes the release of growth factors, cytokines, and other signaling molecules that coordinate tissue repair processes. The mechanical stimulation also activates fibroblasts, the cells responsible for collagen production, leading to the formation of new, healthy tissue that gradually replaces damaged structures.
Breaking Up Scar Tissue and Calcification
One of the most significant advantages of shockwave therapy is its ability to mechanically disrupt pathological tissue formations that impede normal function. Chronic injuries often involve the formation of dense scar tissue, adhesions, and calcific deposits that create mechanical restrictions and pain. The acoustic waves generated during treatment create sufficient mechanical stress to break down these formations without damaging surrounding healthy tissue. Using shockwaves, we can apply targeted force inside the bone to create small cavities in which a hematoma – a pool of blood, similar to a bruise – can form. This principle applies to soft tissues as well, where the controlled disruption of scar tissue allows for the formation of new, more functional tissue with improved mechanical properties. The breakdown of calcifications and adhesions restores normal tissue mobility and reduces mechanical irritation that contributes to chronic pain.
Reducing Pain Without Medication
The analgesic effects of shockwave therapy occur through multiple mechanisms that provide both immediate and long-term pain relief without the need for pharmaceutical interventions. The mechanical stimulation of nerve fibers creates a temporary disruption in pain signal transmission, providing immediate relief during and after treatment sessions. This effect is based on the gate control theory of pain, where non-painful stimuli can inhibit the transmission of pain signals to the brain. Long-term pain reduction occurs through the normalization of tissue structure and function, which eliminates the underlying sources of nociceptive input. The improved tissue quality, enhanced vascularization, and reduced inflammation that result from shockwave therapy address the root causes of chronic pain rather than merely masking symptoms. Additionally, the therapy has been shown to influence substance P levels and other pain mediators, creating lasting changes in pain perception and sensitivity.
Improving Mobility and Performance
The functional improvements achieved through shockwave therapy extend beyond pain reduction to include enhanced range of motion, improved tissue elasticity, and restored biomechanical function. These improvements occur through the remodeling of scar tissue, normalization of tissue architecture, and enhancement of cellular metabolism. The mechanical properties of treated tissues gradually improve as new collagen formation creates stronger, more elastic structures. The enhancement of tissue vascularization through neovascularization also contributes to improved function by ensuring adequate oxygen and nutrient delivery to previously compromised areas. This improved blood supply supports ongoing tissue maintenance and repair processes, reducing the likelihood of future injury recurrence. Many athletes report not only resolution of chronic pain but also improved performance capabilities that may exceed pre-injury levels.
Common Old Sports Injuries Treated with Shockwave Therapy
Shockwave therapy has demonstrated particular effectiveness in treating specific chronic conditions that commonly affect athletes and active individuals. Understanding these applications helps identify appropriate candidates for treatment.
Chronic Achilles Tendinopathy
Chronic Achilles tendinopathy represents one of the most challenging conditions in sports medicine, often resisting conventional treatment approaches for months or years. Achilles tendinopathy is characterized by pain and swelling in the Achilles tendon, often resulting from overuse or injury. ESWT stimulates tendon repair and reduces pain, making it particularly effective for this condition. The treatment addresses the degenerative changes in tendon structure that characterize chronic tendinopathy, including collagen disorganization and neovascularization. The effectiveness of shockwave therapy for Achilles tendinopathy stems from its ability to stimulate tenocyte proliferation and promote the synthesis of high-quality collagen fibers. The mechanical stimulation breaks down pathological tissue formations while simultaneously promoting the regeneration of healthy tendon tissue. Many athletes experience significant improvement in pain levels and functional capacity, allowing for gradual return to training and competition activities.
Fascitis plantar That Never Went Away
Chronic plantar fasciitis represents one of the most well-documented applications of shockwave therapy, with extensive research demonstrating its effectiveness. In the United States, an FDA study was performed for patients who suffer from chronic plantar fasciitis with or without the presence of a heel spur. The results were an amazing average reduction in pain of 92% with only one treatment. This remarkable success rate has made shockwave therapy a preferred treatment for recalcitrant plantar fasciitis cases. The therapy works by addressing the chronic inflammatory changes and thickening of the plantar fascia that characterize this condition. The mechanical disruption of pathological tissue formations, combined with the stimulation of healing processes, leads to normalization of fascial thickness and improved tissue quality. The treatment is particularly effective for cases involving heel spurs, where the mechanical forces can help break down calcific deposits that contribute to pain and dysfunction.
Codo de tenista y Golfer’s Elbow
Lateral epicondylitis (tennis elbow) and medial epicondylitis (golfer’s elbow) are common chronic conditions that respond well to shockwave therapy. For lateral epicondylitis (LE), the SMD was 0.63 (SMD: -0.63, 95% CI: -1.11, -0.16; I2: 67.50%; P heterogeneity: 0.003). These conditions involve degenerative changes in the tendon attachments at the elbow, creating persistent pain and functional limitations that can significantly impact both athletic performance and daily activities. The treatment addresses the underlying tendinopathy by stimulating cellular regeneration and improving the structural integrity of the affected tendons. The mechanical forces generated during treatment help break down scar tissue and calcifications that contribute to pain and restricted movement. Many patients experience significant improvement in grip strength and pain levels, allowing for gradual return to sports activities and improved quality of life.
Tendinopatía rotuliana (Jumper’s Knee)
Patellar tendinopathy, commonly known as jumper’s knee, is a chronic condition that particularly affects athletes involved in jumping and running sports. The condition involves degenerative changes in the patellar tendon, leading to persistent pain and functional limitations that can be career-threatening for competitive athletes. Shockwave therapy has shown particular promise in treating this condition by addressing the underlying pathological changes in tendon structure. The treatment stimulates the regeneration of healthy tendon tissue while breaking down the pathological formations that characterize chronic tendinopathy. The mechanical stimulation promotes cellular proliferation and collagen synthesis, leading to improved tendon quality and function. Many athletes report significant improvements in pain levels and jumping performance, allowing for successful return to competitive activities.
Hamstring and Groin Strains
Chronic hamstring and groin strains represent complex injuries that often involve multiple tissue types and can be particularly challenging to treat effectively. These injuries frequently involve both muscular and tendinous components, creating complicated patterns of pain and dysfunction that may persist for months or years. Shockwave therapy addresses these complex injuries by promoting tissue healing and breaking down restrictions that impede normal function. The treatment is particularly effective for addressing the formation of scar tissue and adhesions that commonly develop following hamstring and groin injuries. The mechanical forces generated during treatment help restore normal tissue architecture and improve the mechanical properties of injured structures. Many athletes experience improved flexibility, reduced pain, and enhanced performance capabilities following treatment.
Qué esperar durante y después de la terapia con ondas de choque
Understanding the treatment process and recovery timeline helps patients prepare for therapy and optimize their outcomes. The experience of shockwave therapy is generally well-tolerated and involves minimal disruption to daily activities.
The Treatment Session
A typical shockwave therapy session lasts approximately 15-20 minutes and begins with a thorough assessment of the injured area to determine optimal treatment parameters. The skin is prepared with ultrasound gel to ensure proper acoustic coupling, and the shockwave applicator is positioned directly over the treatment area. The intensity is gradually increased to therapeutic levels while monitoring patient comfort and response. During treatment, patients typically experience a pulsing sensation that may range from mild discomfort to moderate intensity, depending on the condition being treated and individual pain tolerance. The sensation is generally described as tolerable and brief, lasting only during the actual pulse delivery. Treatment parameters are adjusted based on patient response and the specific condition being addressed, ensuring optimal therapeutic benefit while maintaining patient comfort.
Aftercare and Recovery Timeline
Following shockwave therapy, patients may experience mild soreness or swelling in the treated area, which typically resolves within 24-48 hours. Ice application and over-the-counter pain relievers can be used to manage any discomfort, though most patients require minimal post-treatment care. Activity modification may be recommended for the first few days following treatment to allow optimal tissue response to the therapy. The recovery timeline varies depending on the specific condition being treated and individual healing factors. Many patients begin experiencing improvements within 2-4 weeks of treatment, with continued progress over the following 8-12 weeks. The full benefits of treatment may not be apparent until 3-6 months post-treatment, as tissue remodeling and healing processes continue long after the initial therapy sessions.
Success Rates and Patient Testimonials
The success rate ranged from 65% to 91%, and the complications were low and negligible. These impressive success rates reflect the effectiveness of shockwave therapy across various chronic conditions. The average pain level before treatment was 7.7. After receiving one ESWT treatment, the patients were asked one year later to rate their pain level again on a scale of 1 to 10. The patients who reported had an average pain score post-ESWT of 0.6. This is a 92% reduction in pain, demonstrating the long-lasting benefits of this treatment approach. Patient testimonials consistently highlight the life-changing impact of successful shockwave therapy treatment. Many report not only significant pain reduction but also improved function, enhanced quality of life, and successful return to athletic activities. The non-invasive nature of the treatment and minimal recovery time make it particularly appealing to athletes who cannot afford extended periods away from training and competition.

Contraindicaciones y consideraciones
While shockwave therapy is generally safe and well-tolerated, certain conditions and circumstances require careful consideration or may preclude treatment. Understanding these limitations ensures appropriate patient selection and optimal safety outcomes.
Who Should Not Receive ESWT?
Absolute Contraindications:
Pregnancy – risk to fetal development.
Cardiac pacemakers or implanted electrical devices – potential interference.
Malignant tumors in or near the treatment area – risk of stimulating tumor growth.
Bleeding disorders or active anticoagulant therapy – increased risk of hematoma or internal bleeding.
Relative Contraindications:
Open wounds or skin infections at the treatment site.
Compromised skin integrity, including ulcers or dermatitis.
Severe osteoporosis – fragile bones may be more prone to microfracture.
Certain neurological disorders, such as epilepsy or sensory neuropathies.
Medications that affect healing or pain sensitivity.
Growth plates in children or adolescents – risk to bone development.
Posibles efectos secundarios
Mild pain or discomfort during treatment.
Redness or swelling at the treatment site.
Bruising or minor skin irritation.
Temporary numbness or tingling, especially near nerves.
Slight worsening of symptoms in the short term (rare).
Enhancing Recovery with Supportive Strategies
Maximizing the benefits of shockwave therapy often involves combining treatment with complementary approaches that support healing and prevent future injury recurrence. These strategies create a comprehensive treatment plan that addresses multiple aspects of recovery.
Pairing with Physical Therapy and Rehab
The combination of shockwave therapy with structured physical therapy and rehabilitation programs creates synergistic effects that enhance treatment outcomes. Physical therapy provides the movement patterns and strengthening exercises necessary to restore normal function and prevent future injury recurrence. The improved tissue quality achieved through shockwave therapy creates optimal conditions for effective rehabilitation exercises. The timing of physical therapy initiation relative to shockwave treatment requires careful coordination to optimize benefits while avoiding interference with healing processes. Generally, gentle mobility exercises can be initiated immediately following treatment, with progressive strengthening and functional training introduced as tissue healing progresses. This integrated approach addresses both the structural improvements achieved through shockwave therapy and the functional requirements necessary for successful return to athletic activities.
Role of Nutrition and Hydration
Proper nutrition and hydration play crucial roles in supporting the healing processes stimulated by shockwave therapy. Adequate protein intake provides the building blocks necessary for collagen synthesis and tissue repair, while specific nutrients such as vitamin C, zinc, and omega-3 fatty acids support healing processes. Anti-inflammatory foods can help modulate the inflammatory response and support optimal tissue remodeling. Hydration is particularly important for maintaining optimal tissue metabolism and supporting the elimination of cellular debris generated during treatment. Adequate fluid intake also helps maintain optimal blood flow to treated areas, ensuring delivery of nutrients and oxygen necessary for healing processes. Many practitioners recommend specific nutritional strategies to optimize treatment outcomes and support long-term tissue health.
Preventing Future Relapses
Long-term success following shockwave therapy depends on addressing the underlying factors that contributed to the initial injury development. This includes correcting biomechanical abnormalities, addressing training errors, and implementing appropriate load management strategies. Regular assessment of movement patterns and functional capacity helps identify potential problems before they lead to symptom recurrence. Ongoing maintenance strategies may include periodic preventive treatments, continued conditioning programs, and regular monitoring of tissue health through imaging studies or functional assessments. Education about proper training techniques, equipment selection, and injury prevention strategies helps athletes maintain the benefits achieved through treatment and reduce the risk of future injury development.
Conclusion: Old Injuries, New Hope
Marcas de la terapia de ondas de choque a turning point for athletes and active individuals struggling with chronic sports injuries. Unlike conventional treatments that often mask symptoms, ESWT targets the root causes—stimulating healing, breaking down scar tissue, and restoring normal function. With impressive success rates, minimal side effects, and no need for surgery or downtime, it’s quickly becoming a go-to solution in sports medicine. This non-invasive approach activates the body’s natural repair systems, making it ideal for conditions that have resisted rest, medication, or physical therapy. As ongoing research uncovers new applications and refines treatment protocols, the potential for even broader use continues to grow. For many, shockwave therapy delivers more than just pain relief—it offers real healing and a return to peak performance. In a landscape where chronic injuries once meant compromise, ESWT brings renewed hope—and the sound of recovery is making waves.
FAQs About Shockwave Therapy for Old Injuries
Yes. Even injuries that are years or decades old can respond well. Shockwave therapy reactivates healing by breaking down scar tissue and promoting regeneration. Some cases may require more sessions, but many long-term injuries improve significantly.
Most conditions need 3–6 sessions for results. Some patients don’t need further treatment for years, while others benefit from occasional maintenance—especially if they stay highly active or at risk for reinjury.
Mild to moderate discomfort may occur during the session, often described as tapping or pulsing. Some soreness afterward is normal and usually resolves in 1–2 days, similar to a workout ache.
Some feel relief within 2–4 weeks, while full effects can take up to 12 weeks or longer. Healing continues after sessions end, so patience is key.
Yes, but with modifications. Light activity is usually allowed, but you may need to pause intense or high-impact training temporarily to support healing.
Often, yes. It can treat residual scar tissue or incomplete healing post-surgery—after proper healing time (6–8 weeks). Always consult your surgeon before beginning.
Referencias
- Cómo vence la terapia de ondas de choque a la tendinopatía
- Tratamiento con ondas de choque para las molestias del desgarro del manguito de los rotadores
- Terapia de ondas de choque para la espalda lumbar que funciona
- Cómo la terapia de ondas de choque está transformando la rehabilitación atlética
- Effectiveness of extracorporeal shockwave therapy for chronic Achilles tendinopathy: A randomized clinical trial
The effectiveness of shockwave therapy on patellar tendinopathy, Achilles tendinopathy, and plantar fasciitis: a systematic review and meta-analysis
Eficacia y seguridad de la terapia con ondas de choque en las tendinopatías
