Introduction
Tenosynovitis, a condition marked by inflammation of the tendon sheath, often causes debilitating pain and impaired function in the affected region. This condition can dramatically interfere with an individual’s ability to perform daily tasks, especially those involving fine motor skills or repetitive wrist and finger movements. Traditional treatments like immobilization, anti-inflammatory medications, corticosteroid injections, or surgical intervention come with varying degrees of success and potential side effects. Extracorporeal Shockwave Therapy (ESWT) has emerged as a promising non-invasive treatment option for musculoskeletal disorders, including tenosynovitis. This article explores the scientific basis, therapeutic potential, and practical application of ESWT in managing tenosynovitis, aligning with evidence-based medical standards and Google E-E-A-T (Experience, Expertise, Authoritativeness, and Trustworthiness) principles.
Understanding Tenosynovitis and Its Challenges
Definition and Common Types
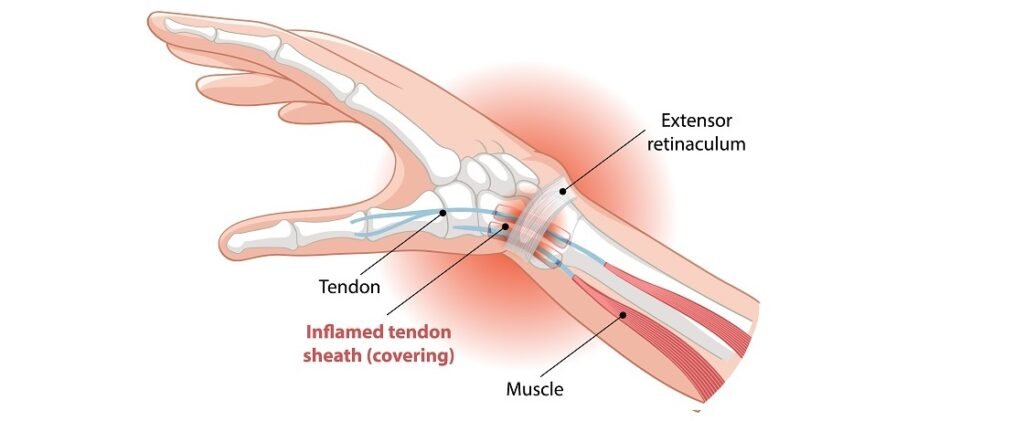
Tenosynovitis refers to the inflammation of the synovial sheath surrounding a tendon. This sheath is responsible for reducing friction between the tendon and surrounding structures during motion. Common types of tenosynovitis include:
- De Quervain’s Tenosynovitis: Affects the tendons on the thumb side of the wrist, often due to repetitive gripping or overuse.
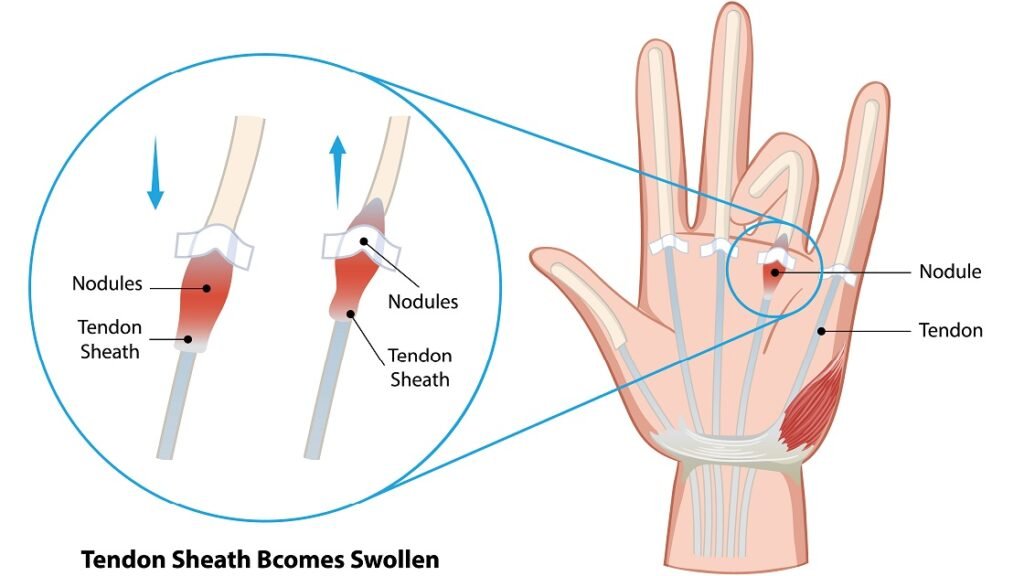
- Trigger Finger (Stenosing Tenosynovitis): Involves inflammation of the flexor tendon sheath in the fingers, causing painful locking or catching.
- Extensor and Flexor Tenosynovitis: Involves tendons in the hands, feet, or ankles, frequently observed in athletes and workers with repetitive hand or foot use.
Root Causes and Mechanisms
The pathophysiology of tenosynovitis primarily involves repetitive mechanical overuse, which leads to microtrauma and subsequent chronic inflammation of the tendon sheath. This persistent irritation induces synovial hyperplasia and the release of pro-inflammatory cytokines such as interleukin-1 and tumor necrosis factor-alpha, which exacerbate tissue damage. In addition to mechanical factors, systemic inflammatory conditions like rheumatoid arthritis, gout, and diabetes mellitus can predispose individuals by compromising tendon integrity and healing capacity. Occasionally, infectious agents cause infectious tenosynovitis, which requires immediate intervention. The interplay of mechanical stress and biochemical inflammation creates a cycle of pain and impaired function, often complicated by fibrosis and adhesions within the sheath, further restricting tendon mobility.
Symptoms That Disrupt Daily Life
Clinically, tenosynovitis manifests as localized tenderness, swelling, warmth, and a palpable crepitus along the tendon sheath. Patients frequently report stiffness, especially after periods of inactivity, and pain that intensifies with specific movements. In trigger finger, this is exemplified by a catching or locking sensation, sometimes requiring manual manipulation to unlock the digit. De Quervain’s tenosynovitis typically causes pain over the radial styloid process, aggravated by thumb movements such as gripping or pinching. These symptoms interfere significantly with activities of daily living, occupational tasks, and hobbies, often leading to decreased hand function and quality of life. Chronic cases can progress to tendon rupture or permanent motion limitations if untreated, underscoring the importance of early diagnosis and effective management.
Risk Factors and High-Risk Groups
Risk factors for tenosynovitis extend beyond repetitive strain to include demographic and medical variables. Women are disproportionately affected, especially during the postpartum period due to hormonal influences on tendon elasticity and fluid retention. Occupations involving repetitive wrist and finger motions—such as musicians, typists, manual laborers, and assembly line workers—are at increased risk. Additionally, aging is associated with degenerative changes in tendon structure and vascular supply, predisposing older adults to tendinopathies. Comorbidities like diabetes impair microvascular circulation and tendon repair mechanisms, exacerbating inflammation and delaying healing. Sports involving repetitive gripping or wrist flexion, such as tennis or golf, also elevate the risk, making tenosynovitis a common overuse injury in athletes.
Shockwave Therapy: A Game-Changer for Tenosynovitis
What is Focused Shockwave Therapy?
Focused Extracorporeal Shockwave Therapy (fESWT) is an advanced, non-invasive treatment modality that delivers high-energy acoustic waves to precise locations within soft tissues. These shockwaves are generated outside the body and focused through specialized applicators to penetrate deep into affected tendon sheaths. Unlike radial shockwave therapy, which disperses energy more superficially, focused ESWT concentrates energy at a defined focal point, allowing for targeted stimulation of pathological tissue. The procedure is typically performed in outpatient settings without anesthesia, requiring multiple sessions spaced over several weeks. The non-surgical nature of fESWT, combined with its ability to target chronic inflammatory sites, positions it as a revolutionary treatment alternative for refractory tenosynovitis cases that have failed conservative management.
Mechanisms: How ESWT Works on Tenosynovitis
The therapeutic effect of ESWT in tenosynovitis is multifaceted, involving mechanical, cellular, and biochemical mechanisms. The acoustic waves induce controlled microtrauma in the affected tissues, triggering a localized healing response. This microtrauma stimulates the release of angiogenic growth factors such as vascular endothelial growth factor (VEGF), promoting neovascularization and increased blood flow to hypoxic tendon areas. Enhanced perfusion facilitates oxygen and nutrient delivery necessary for tissue regeneration. Additionally, ESWT modulates the inflammatory milieu by downregulating pro-inflammatory cytokines (e.g., interleukin-6) and neuropeptides involved in pain transmission, including substance P, thereby reducing pain and swelling. At a cellular level, shockwaves stimulate tenocyte proliferation and collagen synthesis, improving the structural integrity and elasticity of the tendon sheath. These combined effects contribute to symptom relief and functional recovery.
Backed by Science: Clinical Evidence
Numerous clinical studies validate the efficacy of focused ESWT in treating tenosynovitis. For instance, randomized controlled trials investigating its use in De Quervain’s tenosynovitis have demonstrated significant improvements in pain scores, grip strength, and functional outcomes compared to placebo or corticosteroid injections. A recent systematic review and meta-analysis focusing on trigger finger patients revealed that ESWT provides substantial symptom relief and reduces the need for surgical intervention, with minimal adverse effects. Long-term follow-up studies indicate durable benefits with reduced recurrence rates. These findings support ESWT as a safe, evidence-based, and cost-effective alternative or adjunct to traditional therapies, offering renewed hope for patients suffering from chronic tendon sheath inflammation.
Benefits of Shockwave Therapy for Tenosynovitis
Non-Surgical and Minimally Invasive
One of the primary advantages of extracorporeal shockwave therapy (ESWT) is its non-surgical, minimally invasive nature. Unlike traditional surgical interventions, ESWT does not require incisions, anesthesia, or prolonged hospital stays, significantly reducing the risks associated with invasive procedures, such as infections, scarring, and prolonged rehabilitation. This characteristic makes ESWT an appealing option for patients who wish to avoid the complications and downtime linked to surgery. Additionally, because it targets the pathology directly through focused acoustic energy, ESWT offers precise treatment without damaging surrounding tissues. This focused approach facilitates faster healing while minimizing discomfort during and after the procedure.
Quick Recovery and Long-Lasting Relief
ESWT promotes accelerated tissue regeneration and modulates inflammatory processes, allowing patients to experience relatively rapid symptomatic relief. Many patients report a reduction in pain and improved function after just a few treatment sessions, with cumulative benefits increasing over time. Unlike corticosteroid injections, which may offer only temporary relief, ESWT addresses underlying tissue pathology, resulting in more durable outcomes. Clinical studies have demonstrated that the improvements in pain and tendon function can persist for months to years post-treatment, reducing the frequency of recurrent symptoms and the need for further interventions. The relatively short recovery time also enables patients to resume daily activities and return to work or sports much sooner than after surgery.
Reduced Risk of Recurrence
Chronic tenosynovitis often recurs due to persistent mechanical stress and incomplete healing. ESWT reduces this risk by stimulating cellular repair mechanisms, promoting angiogenesis, and restoring normal tendon sheath architecture. By enhancing collagen production and reducing fibrosis, shockwave therapy improves the biomechanical properties of the tendon sheath, increasing its resilience to repetitive strain. Long-term follow-up data show that patients treated with ESWT have a lower incidence of symptom relapse compared to those treated with corticosteroids or conservative measures alone. This suggests that ESWT not only treats symptoms but also modifies disease progression, making it a valuable tool in the long-term management of tenosynovitis.
Improved Mobility and Function
Pain and inflammation in tenosynovitis severely limit joint mobility and functional capacity. ESWT contributes to the restoration of normal tendon glide and joint range of motion by resolving inflammatory swelling and stimulating tendon sheath remodeling. As pain decreases, patients experience enhanced grip strength, dexterity, and overall hand or wrist function, which significantly improves their ability to perform activities of daily living and occupational tasks. For athletes or individuals whose work involves repetitive motions, this functional recovery is crucial for maintaining productivity and preventing disability. The improvement in mobility is often quantifiable through validated clinical scoring systems, such as the Disabilities of the Arm, Shoulder, and Hand (DASH) score, further supporting the objective benefits of ESWT.
High Patient Satisfaction Rates
Patient satisfaction with ESWT is generally very high, attributable to its efficacy, safety profile, and convenience. Because ESWT is outpatient-based, non-invasive, and associated with minimal discomfort, patients often prefer it over injections or surgery. Moreover, the low incidence of side effects—usually limited to transient redness, mild swelling, or discomfort at the treatment site—enhances patient compliance. Surveys and clinical studies report that most patients would recommend ESWT to others suffering from tenosynovitis. The combination of fast pain relief, functional improvement, and avoidance of surgery makes ESWT a preferred treatment option for many individuals, reinforcing its role in modern musculoskeletal care.

Treatment Journey: What Patients Can Expect
Initial Consultation and Diagnosis
The treatment journey with ESWT begins with a comprehensive clinical evaluation by a qualified healthcare provider. During the initial consultation, the physician or therapist will perform a detailed history and physical examination, focusing on symptom duration, severity, and functional limitations. Diagnostic imaging, such as ultrasound or MRI, may be used to confirm tenosynovitis, assess tendon sheath thickness, and exclude other pathologies like tendon tears or joint arthritis. This thorough assessment ensures accurate diagnosis and appropriate treatment planning. Additionally, patients are informed about ESWT’s mechanism, benefits, and potential risks to establish realistic expectations and obtain informed consent.
Treatment Protocol
The standard ESWT protocol for tenosynovitis typically involves multiple sessions, often ranging from three to five treatments spaced one to two weeks apart. Each session lasts approximately 15 to 20 minutes. Focused shockwaves are applied directly over the affected tendon sheath using a specialized probe. Treatment intensity and frequency are tailored based on patient tolerance and severity of symptoms. During the procedure, patients may feel a tapping or tingling sensation, which is generally well-tolerated. The non-invasive nature of ESWT allows patients to remain fully conscious and ambulatory throughout the treatment. Importantly, adjunctive therapies such as physical therapy or ergonomic modifications may be recommended to optimize outcomes.
Post-Treatment Guidelines
After ESWT sessions, patients are advised to avoid strenuous activities that exacerbate symptoms for at least 48 hours to facilitate tissue healing. Mild soreness or localized bruising may occur but usually resolves within days. Over-the-counter analgesics may be used if necessary, though strong pain medications are rarely required. Patients are encouraged to perform gentle range-of-motion exercises as tolerated to maintain mobility. Follow-up appointments help monitor progress, adjust treatment parameters if needed, and reinforce lifestyle modifications to prevent recurrence. Adherence to post-treatment guidelines is crucial for maximizing therapeutic benefits and minimizing complications.
Who Is an Ideal Candidate?
Ideal candidates for ESWT are individuals with chronic, refractory tenosynovitis who have not responded adequately to conservative treatments such as rest, splinting, NSAIDs, or corticosteroid injections. Patients with localized tendon sheath inflammation confirmed by clinical and imaging studies are good candidates. ESWT is particularly beneficial for those seeking to avoid surgery or for whom surgery is contraindicated. Patients with well-controlled systemic inflammatory diseases may also benefit. However, candidacy must be individualized based on the patient’s overall health status, symptom severity, and treatment goals.
Who Should Avoid ESWT?
Despite its favorable safety profile, ESWT is contraindicated in certain populations. Patients with coagulation disorders or those on anticoagulant therapy are at increased risk of bleeding complications and should avoid treatment. Pregnant women are generally excluded due to unknown effects on the fetus. Additionally, patients with active infections or tumors in the treatment area should not undergo ESWT. Caution is advised in individuals with implanted electronic devices, such as pacemakers, as shockwaves could theoretically interfere with device function. A thorough medical history and screening are essential to identify these contraindications and ensure patient safety.
Frequently Asked Questions (FAQ)
Q1: Is shockwave therapy effective for all types of tenosynovitis?
Shockwave therapy is particularly effective for chronic, non-infectious tenosynovitis, especially when conventional treatments have failed. It is less suitable for acute infectious forms, which require antibiotics or surgical drainage. Imaging and clinical evaluation help determine candidacy.
Q2: Is the procedure painful or risky?
Discomfort is generally mild and temporary, similar to a tapping or pulsing sensation. The treatment is non-invasive, so it carries very low risk—with minor side effects like localized redness or swelling that resolve quickly.
Q3: Can I continue normal activities after ESWT sessions?
Yes, you can resume light daily activities immediately. However, it is recommended to avoid intense repetitive motions or heavy exercise for 48–72 hours to allow tissue recovery.
Q4: Will I need repeated treatments in the future?
Most patients experience long-lasting relief after one treatment cycle. However, if underlying risk factors persist (e.g., repetitive strain at work), maintenance sessions may be needed. Preventive ergonomics and stretching can reduce recurrence.
Q5: Are there any people who should not receive ESWT?
Yes. Shockwave therapy is not recommended for individuals who are pregnant, have bleeding disorders, use blood thinners, or have tumors, infections, or open wounds at the treatment site. Proper medical screening is essential.
Q6: Can ESWT replace surgery for tenosynovitis?
In many chronic cases, yes. ESWT offers a non-surgical alternative that resolves symptoms without anesthesia, incisions, or long recovery times. For patients reluctant to undergo surgery or unfit for it, ESWT is often a preferred choice.
Expert Opinions and Future Potential
What Clinicians and Therapists Say
Medical professionals increasingly recognize extracorporeal shockwave therapy (ESWT) as a valuable, non-invasive option for treating tenosynovitis. Orthopedic specialists and physical therapists alike have praised its efficacy, especially in cases resistant to conservative therapies like NSAIDs, rest, and corticosteroid injections. Clinicians report that ESWT not only reduces pain but also shortens recovery time, allowing patients to return to daily activities sooner than with traditional methods. Importantly, practitioners emphasize its role as a functional intervention—meaning it addresses both symptoms and the underlying tissue dysfunction. Physical therapists note improvements in grip strength, range of motion, and tendon elasticity after just a few sessions. Furthermore, for conditions like De Quervain’s and trigger finger, ESWT is now often recommended before considering surgical options.
Emerging Applications of ESWT in Tendon Disorders
Shockwave therapy is already well-established for conditions like plantar fasciitis and calcific tendinopathy. Now, its use in tendon and tendon sheath disorders is expanding rapidly. Studies are evaluating its role in treating lateral and medial epicondylitis (tennis and golfer’s elbow), rotator cuff tendinopathy, patellar tendinopathy, and Achilles peritendinitis. These conditions share key pathophysiological features with tenosynovitis—such as chronic inflammation, microtrauma, and fibrosis. All of these factors respond well to shockwave stimulation. Researchers are also exploring ESWT as a preventive strategy for athletes and high-risk workers. The goal is to enhance collagen remodeling and reinforce tendon structures before symptoms develop. Meanwhile, advances in focused and radial wave technology are improving precision and reducing treatment durations.
Need for More Research
Despite its growing clinical use, more high-quality randomized controlled trials are still needed. These studies can help standardize treatment protocols and assess long-term efficacy across different types of tenosynovitis. Current literature shows wide variation in energy levels, treatment sessions, and outcome measures, which makes comparison difficult. Early results are promising, especially for subtypes like De Quervain’s tenosynovitis. However, evidence remains limited for conditions involving the flexor sheath or extensor compartments. Long-term studies are also necessary to track recurrence rates and define any necessary maintenance schedules. Additionally, combining ESWT with other treatments—such as ultrasound-guided injections or platelet-rich plasma (PRP)—may offer added benefits. Still, more data is required to confirm the value of these combined approaches.
Conclusion
Extracorporeal shockwave therapy represents a paradigm shift in the non-invasive treatment of tenosynovitis. By harnessing mechanical energy to stimulate biological healing, it provides a multifaceted solution—reducing inflammation, promoting tissue regeneration, and enhancing tendon function without surgery. Clinical evidence supports its use for stubborn, chronic cases, especially where other treatments have failed. With rapid recovery times, minimal side effects, and growing clinician endorsement, ESWT stands at the forefront of modern musculoskeletal care. As research continues to evolve, this therapy may soon become the standard of care for a broad spectrum of tendon disorders, helping more patients return to pain-free living. For those battling the frustrating limitations of tenosynovitis, shockwave therapy offers not just relief—but renewed hope.
References
The Effect of Extracorporeal Shockwave Therapy on de Quervain Tenosynovitis; a Clinical Trial
