Myofascial Pain Syndrome (MPS) is a chronic condition characterized by pain and inflammation in the body’s soft tissues. Traditional treatments often include medications, physical therapy, and injections. However, advancements in medical technology have introduced Shockwave Therapy as a non-invasive and effective alternative. This guide delves into the causes of MPS, the science behind Shockwave Therapy, its benefits, procedure, clinical evidence, potential side effects, and the standout features of the Swave-200 device.
Causes of Myofascial Pain
Myofascial Pain Syndrome (MPS) is a chronic pain disorder characterized by the presence of myofascial trigger points (MTrPs)—hyperirritable nodules located within taut bands of skeletal muscle. These trigger points can produce referred pain, muscle stiffness, and motor dysfunction. Primary causes of MPS include:
- Muscle Overuse or Repetitive Strain: Repetitive motions, such as prolonged typing or heavy lifting, can cause microtrauma in muscle fibers. This repetitive strain can lead to persistent trigger point formation and localized ischemia (poor blood flow).
- Direct Trauma or Injury: Blunt force injuries or whiplash can disrupt the normal function of muscle tissue, resulting in chronic trigger point activation.
- Postural Imbalances: Poor posture—such as slouching at a desk or uneven gait—leads to muscular imbalances. These strain certain muscle groups disproportionately, promoting myofascial dysfunction.
- Stress and Psychological Factors: Emotional stress can increase muscle tension and elevate levels of cortisol, a hormone known to impair muscle recovery and increase pain sensitivity.
- Systemic Conditions: Fibromyalgia, hypothyroidism, vitamin D deficiency, and chronic infections may predispose patients to myofascial pain through complex neurochemical and muscular pathways.

How Do Shockwaves Treat Myofascial Pain?
Shockwave therapy addresses myofascial pain by targeting both the mechanical dysfunction and the neurochemical imbalances contributing to trigger point development. The core mechanism involves the delivery of high-energy acoustic pulses to affected tissues, promoting regeneration, reducing inflammation, and inhibiting pain signaling pathways.
The Mechanical and Acoustic Principles Behind Shockwaves
Shockwaves used in therapy are categorized as extracorporeal shockwaves—high-pressure acoustic waves that propagate through tissue at supersonic speeds. These waves are delivered in either focused or radial forms:
- Focused Shockwaves (fESWT): High-intensity, deep-penetrating waves targeting precise myofascial trigger points.
- Radial Shockwaves (rESWT): Disperse over a broader surface area with lower energy, ideal for superficial muscle layers.
The mechanical pressure from shockwaves generates shear forces, leading to:
- Microtrauma and cavitation: Controlled tissue stress that triggers repair mechanisms.
- Increased local perfusion: Promotes oxygenation and nutrient delivery.
- Lysis of fibrotic adhesions: Breaks down dysfunctional collagen matrices and restores elasticity.
Disrupting the Pain Pathway
Myofascial pain is maintained by persistent input from nociceptors and dysfunctional motor end plates in trigger points. Shockwave therapy disrupts this process through several mechanisms. The mechanical stimulus of shockwaves converts into biological signals that ultimately decrease central sensitization—a hallmark of chronic myofascial pain:
- Desensitization of Aδ and C-fibers: Acoustic pulses temporarily overload pain-transmitting nerve fibers, reducing their excitability.
- Inhibition of Substance P: A neuropeptide central to pain perception and neurogenic inflammation, Substance P levels drop significantly post-treatment.
- Neuromodulation: Alters the central processing of pain in the spinal cord and brainstem, leading to long-term changes in pain perception.
Neurological and Biochemical Benefits
In addition to disrupting pain pathways, shockwave therapy delivers profound neurological and biochemical advantages:
- Nitric Oxide (NO) Surge: NO acts as a vasodilator and neuromodulator. Its release increases blood flow and decreases pain sensitivity.
- Growth Factor Upregulation: Vascular endothelial growth factor (VEGF), insulin-like growth factor (IGF), and bone morphogenetic proteins (BMPs) are stimulated, enhancing tissue regeneration.
- Decreased Pro-inflammatory Cytokines: IL-6 and TNF-α, two cytokines elevated in myofascial pain, are downregulated post-treatment.
- Endorphin Release: Encourages natural analgesia via endogenous opioids.
These changes promote an environment conducive to muscle healing, nerve repair, and pain resolution—all without pharmacological intervention.
Benefits of Shockwave Therapy for Myofascial Pain
The therapeutic value of shockwave therapy lies in its ability to provide effective, non-invasive, and long-lasting relief for chronic muscle pain.
Natural Pain Relief Options
Unlike medications that mask symptoms or injections that carry systemic risks, shockwave therapy offers drug-free pain relief. It does so by:
- Targeting the root cause—the trigger point—rather than just modulating perception.
- Stimulating intrinsic repair mechanisms, such as collagen remodeling and vascularization.
- Minimizing the reliance on painkillers, thereby reducing risks of side effects, addiction, or tolerance.
A meta-analysis published in Clinical Rehabilitation (2021) reported that patients experienced significant reductions in pain scores (up to 60–80%) after three to five sessions, outperforming many conservative treatments.
Improved Mobility and Muscle Function
Myofascial pain often restricts range of motion, impairs motor control, and leads to compensatory movement patterns. Shockwave therapy restores normal muscle function by breaking down myofascial adhesions, improving fascial glide, and relaxing hypertonic fibers. Clinical improvements include increased flexibility, better joint mobility, and reduced muscle stiffness—particularly in the neck, shoulder, lower back, and calves. This makes it a preferred option for athletes and manual laborers alike.
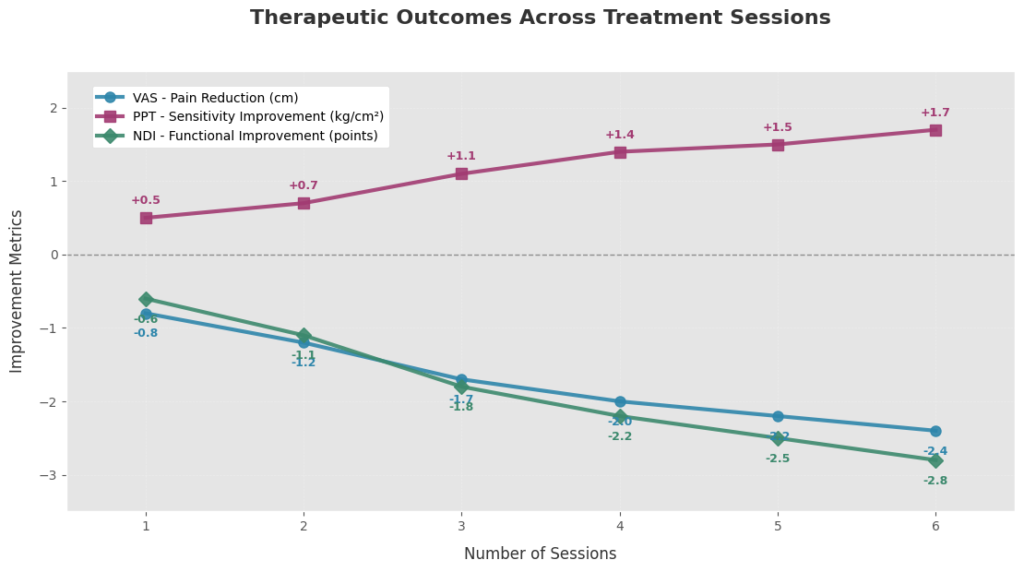
Lasting Results with Fewer Sessions
Unlike massage therapy or TENS units, which often require frequent maintenance treatments, shockwave therapy delivers long-term benefits in a short treatment window. This efficiency not only lowers the overall cost of care but also increases compliance and patient satisfaction:
Typical protocol: 3–6 sessions spaced one week apart.
Duration of relief: Up to 6–12 months in many cases.
Cumulative effect: Each session builds on the last, progressively reducing symptoms.

The Shockwave Therapy Procedure
Shockwave therapy is a non-invasive outpatient procedure that requires minimal preparation and downtime. Here’s what patients and clinicians can expect during each stage.
Pre-Treatment Evaluation
Effective treatment begins with a thorough clinical workup to identify the source and severity of myofascial pain. This includes:
- History Taking: Assessing duration, location, and intensity of symptoms.
- Palpation of Trigger Points: Identifying tender nodules, referred pain patterns, and local twitch responses.
- Functional Testing: Evaluating range of motion, muscle strength, and gait abnormalities.
- Imaging (if needed): Musculoskeletal ultrasound or MRI may be used to confirm diagnosis or rule out structural causes.
What Shockwave Therapy Feels Like
The treatment duration is short, ranging from 10–15 minutes depending on the area and condition. The treatment itself is generally well-tolerated. Patients often describe the sensation as:
- “Tapping” or “pulsing” against the skin
- A mild ache that decreases as the trigger point becomes desensitized
- Occasionally, a brief spike in discomfort when the wave hits an active trigger point (a positive indicator of correct localization)
Each session involves:
- Application of a conductive gel
- Use of a shockwave applicator head targeting affected muscles
- Delivery of 1,500 to 3,000 pulses at adjustable frequencies (typically 8–12 Hz)
Aftercare and Recovery Guidelines
Post-procedure care is simple but important for enhancing outcomes:
- Hydration: Aids in clearing metabolic waste released during therapy.
- Rest: Avoid intense physical activity for 24–48 hours.
- Gentle stretching: Maintains gains in flexibility and reduces soreness.
- Observation: Mild bruising, redness, or tenderness may occur and typically resolves in 1–2 days.
Patients are advised to report persistent pain or unusual symptoms, though adverse effects are rare when administered by trained clinicians.
Proven Success of Shockwave Therapy
Scientific Studies Supporting Efficacy
Numerous peer-reviewed studies have validated the use of shockwave therapy for managing myofascial pain. Clinical trials published in journals like Pain Medicine and Archives of Physical Medicine and Rehabilitation have demonstrated significant pain reduction and improved muscle elasticity after three to six sessions. A 2020 meta-analysis found that both focused and radial shockwaves achieved a statistically significant decrease in pain scores compared to placebo, with effects lasting up to 12 weeks post-treatment. The mechanism—disrupting trigger point activity and improving perfusion—has been consistently observed across populations with chronic neck, shoulder, and back myofascial pain syndromes.
Case Studies and Real Patient Stories
Real-world cases offer compelling evidence for shockwave therapy’s impact. One example involves a 45-year-old office worker with chronic trapezius myofascial pain who reported 80% pain relief after four weekly sessions, with mobility and sleep quality significantly improved. Another case features a competitive cyclist experiencing deep gluteal trigger points who regained full training capacity following six sessions of radial shockwave therapy. Patients often report not only physical relief but also enhanced psychological wellbeing, as reduced pain improves mood, focus, and daily function. These stories reinforce the real-life benefits beyond clinical data.
Comparisons with Other Modalities
Compared to manual therapy, dry needling, or TENS units, shockwave therapy provides deeper tissue penetration and longer-lasting relief with fewer sessions. While massage offers temporary muscle relaxation, shockwave therapy actively breaks down trigger point fibrosis and stimulates biological repair. Unlike corticosteroid injections, which carry risks of tissue atrophy and systemic side effects, shockwaves are non-invasive and free of pharmaceutical burden. Moreover, patients typically see faster recovery than with acupuncture or ultrasound, positioning shockwave therapy as both a frontline and adjunctive option in modern musculoskeletal care.
Possible Side Effects and Contraindications
Common and Temporary Side Effects
Shockwave therapy is generally safe when applied by trained professionals, though mild side effects may occur. Patients may experience transient redness, swelling, or bruising at the treatment site due to increased blood flow and minor capillary stress. Temporary soreness or discomfort similar to post-exercise muscle fatigue is common within the first 24–48 hours. These effects are self-limiting and usually resolve without intervention. Adherence to post-treatment hydration and rest often minimizes these symptoms and enhances therapeutic benefit.
Who Should Avoid Shockwave Therapy?
Despite its safety profile, shockwave therapy is not suitable for everyone. It is contraindicated in individuals with blood clotting disorders, active malignancies in the treatment area, or those taking anticoagulant medications. Pregnant patients and individuals with pacemakers or metallic implants near the target zone should avoid the procedure due to potential interference with medical devices or risk of tissue damage. Patients with acute inflammation, open wounds, or active infections at the site of application should also defer treatment until these issues are resolved.
When to Seek Medical Advice
While adverse reactions are rare, patients should consult their clinician if they experience persistent or worsening pain, prolonged swelling, numbness, or signs of infection following treatment. These may indicate an unrelated musculoskeletal issue or improper application. Pre-treatment screening and follow-up evaluations help mitigate such risks. Clinicians should also re-evaluate therapy effectiveness if the patient sees no improvement after several sessions, as an alternative diagnosis or complementary treatment may be needed.
Why Swave-200 Outshines Others?
The Swave-200 stands out in the competitive field of shockwave therapy devices due to its advanced technology, precision engineering, and user-friendly design. It delivers both radial and focused shockwaves with customizable frequency, energy, and pulse parameters—allowing clinicians to tailor treatments based on tissue depth and sensitivity. Unlike many entry-level devices, the Swave-200 integrates intelligent feedback systems that monitor tissue resistance in real time, ensuring safe and effective energy delivery. Its lightweight handpiece, quiet operation, and ergonomic interface reduce clinician fatigue and enhance patient comfort. The Swave-200 also boasts a robust build with minimal maintenance requirements, making it a cost-effective choice for high-volume practices. Its proven outcomes in clinical settings, backed by CE and FDA compliance, solidify its reputation as a premium option for myofascial pain management. Click here to learn more about Swave-200.
Quick Facts about Shockwave Therapy for Myofascial
Q1: Is shockwave therapy just a fancy massage?
A1: Not even close. While both aim to release muscle tension, shockwave therapy uses focused acoustic pulses to penetrate deep into tissue, targeting stubborn trigger points that hands can’t reach. It’s like upgrading from analog to digital.
Q2: Can it really “reset” tight muscles?
A2: Yes! Think of your muscles like a frozen computer. Shockwaves act like a hard reboot—stimulating cellular repair, breaking fibrosis, and restoring normal muscle tone, all without surgery or drugs.
Q3: Why does it work for chronic cases when nothing else does?
A3: Chronic myofascial pain often involves microcirculatory blockages and nerve hypersensitivity. Shockwave therapy improves neovascularization, restores oxygen delivery, and resets abnormal nerve signals, helping break the chronic pain loop.
Q4: Is this the same technology used for kidney stones?
A4: Sort of! The original shockwave tech (lithotripsy) broke kidney stones. The newer, low- to medium-energy shockwave systems used for myofascial pain are gentler but based on the same physics—mechanical stimulation through acoustic energy.
Q5: Can shockwave therapy “wake up” lazy muscles?
A5: Yes. It activates satellite cells and neuromuscular pathways, especially in areas of inhibited muscle function. This “neuro-muscular reset” helps improve strength, posture, and muscle firing patterns after injury or prolonged pain.
Q6: What’s one thing people get wrong about shockwave therapy?
A6: That it’s only for bones and tendons. In reality, myofascial trigger points are among its most responsive targets, especially in the neck, shoulders, lower back, and jaw muscles (TMJ).
Q7: Is there any “cool factor” to the devices used?
A7: Absolutely. The Swave-200, for example, uses precision-controlled pneumatic pulses, ergonomic handpieces, and preloaded pain protocols. It’s like having a smart assistant for myofascial recovery, not just a machine.
Q8: How do athletes and biohackers use it?
A8: Many elite athletes and wellness clinics use it not just to relieve pain, but to optimize muscle recovery, reduce inflammation post-training, and prevent trigger point buildup. It’s now a biohacking tool, not just a therapy.
References
Usefulness of Extracorporeal Shockwave Therapy on Myofascial Pain Syndrome:
https://pmc.ncbi.nlm.nih.gov/articles/PMC8435462
The Effect of Extracorporeal Shock Wave Therapy on Myofascial Pain Syndrome:
https://www.e-arm.org/journal/view.php?number=179
Update on the efficacy of extracorporeal shockwave treatment for myofascial pain syndrome and fibromyalgia:
https://www.sciencedirect.com/science/article/pii/S1743919115011954
