Introduction
Osgood-Schlatter disease represents one of the most common causes of knee pain in adolescents, particularly affecting young athletes during periods of rapid growth. This condition, characterized by painful inflammation at the tibial tuberosity, can significantly impact a teenager’s participation in sports, physical education, and daily activities. As parents and healthcare providers seek effective treatment options that support both symptom relief and healthy development, emerging therapies like extracorporeal shockwave therapy (ESWT) are gaining attention for their potential benefits in managing this challenging condition.
What Is Osgood-Schlatter Disease in Growing Teens?
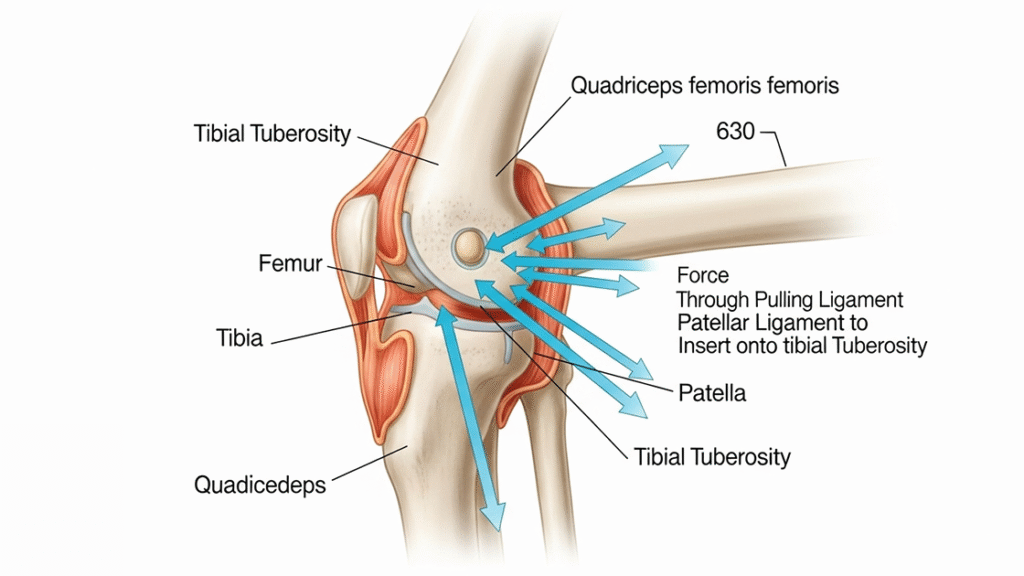
Osgood-Schlatter disease is an apophysitis affecting the tibial tuberosity, where the patellar tendon inserts into the developing tibia. This condition occurs during skeletal growth periods when the apophyseal growth plate remains open and vulnerable to mechanical stress. The immature bone tissue at the tibial tuberosity experiences repetitive traction forces from quadriceps muscle contractions transmitted through the patellar tendon. Up to 10% of adolescents are affected by OSD, making it a significant concern for pediatric and sports medicine practitioners. The condition typically manifests between ages 10-15 years, coinciding with peak growth velocity periods when musculoskeletal imbalances are most pronounced.
Why Choosing the Right Treatment Matters During Growth Spurts
Treatment decisions during adolescent growth spurts require careful consideration of both immediate symptom relief and long-term developmental outcomes. The apophyseal growth plates remain active during this period, making the tibial tuberosity particularly susceptible to overuse injuries and inflammatory responses. Inappropriate treatment approaches may interfere with normal bone development, while inadequate management can lead to chronic pain patterns and activity restrictions. Selecting evidence-based therapies that promote healing while preserving growth plate integrity is crucial for optimal outcomes. The timing of intervention also affects treatment success, as early management typically produces better results than delayed treatment approaches.
Purpose of This Article: Can Shockwave Therapy Help Teen Knee Pain?
This comprehensive analysis examines the potential of shockwave therapy as an effective treatment modality for Osgood-Schlatter disease in adolescents. We will explore current scientific evidence, compare treatment outcomes with conventional approaches, and provide practical guidance for parents and healthcare providers considering this therapeutic option. The article addresses key questions about safety, efficacy, treatment protocols, and integration with other therapeutic interventions. Our goal is to provide evidence-based information that supports informed decision-making about incorporating shockwave therapy into comprehensive treatment plans for young athletes experiencing persistent OSD symptoms despite conventional management approaches.
Understanding Osgood-Schlatter Disease in Adolescents
Comprehensive understanding of Osgood-Schlatter disease pathophysiology, risk factors, and clinical presentation is essential for developing effective treatment strategies. This condition represents a complex interaction between rapid skeletal growth, mechanical stress, and tissue adaptation responses that require specialized management approaches tailored to the unique needs of growing adolescents.
Causes: Growth Spurts, Sports, and Repetitive Stress on the Knee
It is most common during growth spurts in adolescents when bones, tendons, muscles and other structures are changing rapidly, creating mechanical imbalances that predispose to overuse injuries. During peak growth periods, long bone growth typically outpaces muscle-tendon unit elongation, resulting in increased tension across apophyseal attachments. Repetitive quadriceps contractions during running, jumping, and cutting activities generate excessive traction forces at the tibial tuberosity. The immature apophyseal cartilage cannot withstand these repetitive mechanical stresses, leading to microtears, inflammatory responses, and subsequent pain development. Sports requiring frequent jumping, kicking, or sudden directional changes place particular stress on the extensor mechanism, contributing to OSD development in susceptible adolescents.
Common Symptoms: Pain, Swelling, and Tenderness Below the Kneecap
Localized pain at the tibial tuberosity is the hallmark symptom of Osgood-Schlatter disease.
The pain is often described as aching or sharp and worsens with physical activity.
Swelling, warmth, and inflammation commonly accompany the pain around the knee area.
Tenderness on direct pressure over the tibial prominence is nearly universal in affected teens.
Activities like running, stair climbing, or rising from sitting typically intensify discomfort.
A visible bony bump may form at the tibial tuberosity due to reactive bone changes.
Risk Groups: Young Athletes, Active Teens, and Rapid Growth Phases
Adolescents in running, jumping, or contact sports are at higher risk of developing Osgood-Schlatter disease.
Male athletes show slightly higher incidence rates, particularly in explosive lower-body sports.
Basketball, soccer, volleyball, track and field, and gymnastics are high-risk activities.
The condition is most common in ages 10–15, during peak growth velocity.
Rapid growth combined with increased training load raises the likelihood of OSD development.
Individual risk factors include poor quadriceps flexibility, high training intensity, and biomechanical imbalances.
Impact on Daily Life, Sports Participation, and Quality of Life
Osgood-Schlatter disease significantly affects adolescents’ physical function, emotional well-being, and social participation in age-appropriate activities. Pain and discomfort during sports participation often lead to reduced performance levels, missed practices, and potential team exclusion during crucial developmental periods. Academic impacts may include difficulty concentrating due to pain, missed school days for medical appointments, and restricted participation in physical education classes. The condition can affect sleep quality when pain interferes with comfortable positioning, particularly in active adolescents accustomed to regular physical activity. Social and psychological effects include frustration with activity limitations, fear of re-injury, and potential reduction in self-esteem related to decreased athletic performance and peer participation.
Conventional Treatment Approaches
Standard management of Osgood-Schlatter disease traditionally emphasizes conservative interventions focusing on symptom management, activity modification, and supportive care. While these approaches often provide symptomatic relief, their effectiveness in achieving complete resolution varies significantly among individuals, particularly in cases of prolonged or severe symptoms that require more intensive therapeutic interventions.
Rest and Activity Modification: How Much Is Enough?
Complete activity cessation is rarely necessary or recommended for Osgood-Schlatter disease management, as prolonged inactivity may lead to deconditioning and muscle atrophy. Relative rest involves modifying activities to reduce painful symptoms while maintaining cardiovascular fitness and muscle strength. Pain-guided activity modification allows participation in non-aggravating activities while avoiding movements that exacerbate tibial tuberosity discomfort. Cross-training activities such as swimming, cycling, or upper body exercises help maintain fitness levels during symptom management phases. The challenge lies in balancing adequate rest for tissue healing with maintaining physical conditioning and psychological well-being. Activity modification periods typically range from 2-6 weeks, depending on symptom severity and individual response patterns.
Physiotherapy: Stretching and Strengthening for Long-Term Relief
Physiotherapy interventions focus on addressing underlying biomechanical factors contributing to excessive tibial tuberosity stress through targeted exercise programs. Quadriceps and hip flexor stretching helps reduce tension across the patellar tendon-tibial tuberosity complex, potentially decreasing mechanical stress on the apophyseal region. Hamstring flexibility improvements promote better knee mechanics during functional activities, reducing compensatory movement patterns that may exacerbate symptoms. Progressive strengthening exercises targeting the quadriceps, hamstrings, and hip musculature help restore muscle balance and improve force absorption capacity. Core stability training enhances overall movement quality and reduces lower extremity stress during athletic activities. Manual therapy techniques may address joint mobility restrictions and soft tissue tension contributing to altered movement patterns.
Medications: Role of NSAIDs in Managing Pain and Inflammation
Nonsteroidal anti-inflammatory drugs (NSAIDs) serve as first-line pharmacological intervention for managing acute pain and inflammation associated with Osgood-Schlatter disease. Ibuprofen and naproxen are commonly prescribed due to their analgesic and anti-inflammatory properties, helping reduce tibial tuberosity swelling and discomfort. However, concerns about NSAID effects on bone healing and growth plate development limit their long-term use in adolescents. Topical anti-inflammatory preparations may provide localized relief with reduced systemic exposure, making them preferable for younger patients. Acetaminophen offers analgesic benefits without anti-inflammatory effects, providing an alternative for pain management when NSAIDs are contraindicated. Medication use should be combined with other therapeutic interventions rather than serving as the sole treatment approach for optimal outcomes.
Supportive Options: Bracing, Taping, and Ice Therapy
Patellar tendon straps or infrapatellar bracing can help redistribute forces across the tibial tuberosity, potentially reducing localized stress during activities. Kinesiology taping applications may provide proprioceptive feedback and mechanical support while allowing continued participation in modified activities. Ice therapy following activity helps manage acute inflammatory responses and provides temporary pain relief through neurological mechanisms. Heat applications before activity may improve tissue flexibility and reduce stiffness, though ice remains preferred for post-activity inflammation management. Protective padding over the tibial tuberosity helps prevent direct trauma during contact activities or kneeling positions. These supportive measures work best when combined with other therapeutic interventions as part of comprehensive treatment plans rather than standalone interventions.
Limitations of Traditional Care in Persistent Cases
Conventional treatment approaches may prove inadequate for adolescents with severe or persistent symptoms that do not respond to standard conservative management. Some cases require treatment duration extending beyond typical growth periods, creating challenges for young athletes seeking timely return to sports participation. Traditional approaches may not adequately address underlying tissue healing deficits or chronic inflammatory processes contributing to symptom persistence. The passive nature of many conventional treatments may not provide sufficient stimulus for tissue adaptation and repair processes. Complex cases involving multiple contributing factors may require more intensive interventions to achieve satisfactory outcomes. These limitations have prompted investigation of adjunctive therapies such as shockwave treatment to enhance conventional management approaches.
Qu'est-ce que la thérapie par ondes de choc ?
Thérapie extracorporelle par ondes de choc represents an innovative non-invasive treatment modality that utilizes acoustic waves to stimulate tissue healing and pain reduction. Understanding the fundamental principles, mechanisms of action, and safety profile of this technology is essential for healthcare providers and families considering its application in adolescent populations with musculoskeletal conditions.
How Shockwave Therapy Works for Musculoskeletal Pain
Extracorporeal shockwave therapy delivers high-energy acoustic pulses to targeted tissues through specialized applicators that generate controlled mechanical stress waves. These acoustic waves create cavitation effects within tissues, generating microscopic bubbles that collapse and create secondary mechanical stimuli. The mechanical stress induces cellular membrane permeabilization, enhancing cellular metabolism and triggering various biological cascades. Different shockwave modalities include focused and radial wave systems, each offering unique penetration depths and energy distribution patterns. Treatment parameters such as energy density, pulse frequency, and session duration can be adjusted based on specific clinical indications and patient tolerance. The non-invasive nature eliminates surgical risks while providing targeted therapeutic effects directly to affected tissues.
Mechanisms of Action: Pain Modulation, Blood Flow, and Healing
Shockwave therapy modulates pain through multiple neurological pathways, including gate control theory activation and substance P depletion from nerve terminals. The shock waves applied promote blood flow and stimulate stem cell activity in the tissue providing pain relief while increasing the healing response, creating optimal conditions for tissue repair. Neovascularization occurs through angiogenic growth factor release, improving tissue perfusion and nutrient delivery to healing structures. Cellular proliferation increases through enhanced ATP production and protein synthesis activation, accelerating tissue regeneration processes. Anti-inflammatory effects result from reduced pro-inflammatory mediator production and enhanced anti-inflammatory cytokine release. These combined mechanisms create sustained therapeutic effects that extend beyond immediate treatment periods, supporting long-term healing processes.
Safety and Tolerability in Adolescents
This pilot study demonstrates that radial ESWT is a safe and promising treatment for adolescent athletes with recalcitrant Osgood-Schlatter disease, with excellent tolerability profiles in pediatric populations. Treatment-related adverse events remain minimal, typically limited to temporary skin erythema or mild discomfort during application. The non-invasive nature eliminates infection risks and systemic complications associated with invasive procedures or pharmaceutical interventions. Shockwave therapy was focused only on the apophyses away from the growing epiphyses, ensuring safety for developing skeletal structures. Special considerations for adolescent treatment include modified energy parameters, careful applicator positioning, and appropriate session intervals. Most young patients tolerate treatments well, with the brief session duration minimizing discomfort and promoting treatment adherence.
Can Shockwave Therapy Help Osgood-Schlatter Disease?
The growing body of scientific evidence supporting shockwave therapy’s efficacy in treating Osgood-Schlatter disease provides valuable insights for healthcare providers and families seeking effective treatment options. Recent research demonstrates promising outcomes that warrant serious consideration of this therapeutic modality for adolescents with persistent or severe symptoms.
Clinical Evidence: Studies on Shockwave Therapy for Osgood-Schlatter
ESWT is a potentially safe and effective treatment for apophyseal injuries. It may facilitate an early return to sport activities, according to recent clinical research. The time from treatment initiation to previous activity level was 2 weeks in 14 patients (63.3%), 4 weeks in seven patients (31.8%) and 11 weeks in one patient (4.5%). No adverse events were reported. No recurrence occurred up to 3 months after the last session. (2021) found that in a group of 30 patients with OSD, ESWT significantly improved symptoms and enabled earlier return to sports compared to conventional physiotherapy. These studies demonstrate consistent positive outcomes across different patient populations and treatment protocols, supporting the therapeutic value of shockwave therapy for this condition.
How It Relieves Knee Pain and Supports Healing at the Growth Plate
Shockwave therapy targets the pathophysiological mechanisms underlying Osgood-Schlatter disease through direct effects on inflamed apophyseal tissues. The acoustic waves reduce inflammatory mediator production within the tibial tuberosity region, decreasing local swelling and pain intensity. Enhanced cellular metabolism promotes tissue repair processes while stimulating angiogenesis to improve blood supply to the healing apophysis. Pain modulation occurs through neuroplasticity changes and endorphin release, providing both immediate and sustained analgesic effects. Shockwave therapy for Osgood Schlatters disease promotes blood flow and stimulates stem cell activity in the tissue providing pain relief while increasing the healing response. The mechanical stimulation encourages proper collagen formation and tissue remodeling, supporting long-term structural integrity of the tibial tuberosity region.
Short-Term Relief vs. Long-Term Outcomes in Teenagers
Initial pain reduction typically occurs within 1-2 weeks of treatment initiation, providing rapid symptomatic improvement that enables activity resumption. We have seen significant improvement in pain scores and functional outcomes in patients with OSD treated with shockwave therapy compared to those receiving conventional treatments. Long-term outcomes demonstrate sustained pain relief and functional improvement extending 3-6 months beyond treatment completion in most patients. The tissue healing effects continue developing for several weeks after treatment, with progressive improvements in pain levels and activity tolerance. Recurrence rates remain low when treatment protocols are completed appropriately and combined with activity modification strategies. Most adolescents experience lasting symptom resolution that allows full return to sports and recreational activities without ongoing restrictions or discomfort.
Shockwave Therapy Compared to Physiotherapy Alone
Comparative studies indicate superior outcomes when shockwave therapy is combined with conventional physiotherapy compared to physiotherapy alone. The active tissue healing stimulation provided by shockwave therapy appears to enhance and accelerate the benefits achieved through exercise-based interventions. Treatment timelines are typically shorter with combined approaches, enabling faster return to full activity levels for young athletes. Pain reduction occurs more rapidly with shockwave therapy, improving patient compliance with concurrent exercise programs. However, physiotherapy remains important for addressing biomechanical factors and preventing symptom recurrence through improved movement patterns. The combination approach addresses both acute symptoms and underlying predisposing factors, creating optimal conditions for long-term success and injury prevention.
Benefits of Shockwave Therapy for Teen Athletes
Young athletes face unique challenges when managing Osgood-Schlatter disease, as they must balance symptom management with maintaining fitness levels, skill development, and competitive participation. Shockwave therapy offers several advantages specifically beneficial for this population, supporting both immediate symptom relief and long-term athletic development goals.
Pain Relief and Inflammation Reduction at the Tibial Tuberosity
Targeted shockwave application directly addresses inflammatory processes within the tibial tuberosity apophysis, providing focused therapeutic effects where symptoms originate. The acoustic waves penetrate to appropriate tissue depths, creating mechanical stimulation that reduces pro-inflammatory cytokine production. Localized analgesic effects occur through multiple pain modulation pathways, including nerve conduction changes and endorphin release activation. Swelling reduction is typically noticeable within days of treatment, improving knee appearance and reducing tenderness to touch. The anti-inflammatory effects extend beyond treatment sessions, creating sustained improvement in tissue quality and comfort levels. This targeted approach allows for precise treatment of the affected area while preserving surrounding healthy tissues.
Improved Muscle-Tendon Healing and Knee Function
Shockwave therapy enhances collagen synthesis and tissue remodeling processes within the patellar tendon-tibial tuberosity complex, promoting structural integrity restoration. The mechanical stimulation improves muscle-tendon unit compliance and elasticity, reducing excessive tension across the apophyseal attachment site. Neuromuscular function improvements occur through enhanced proprioceptive feedback and reduced pain-related movement inhibition patterns. Range of motion typically increases as pain decreases and tissue quality improves, allowing for better movement efficiency during activities. Strength improvements often follow pain reduction, as athletes can engage in progressive loading without exacerbating symptoms. The combined effects support overall knee function restoration and improved biomechanical efficiency during sports activities.
Faster Return to Sports and Physical Education
The time from treatment initiation to previous activity level was 2 weeks in 14 patients (63.3%), 4 weeks in seven patients (31.8%), demonstrating the potential for rapid return to activity. This accelerated timeline is particularly valuable for young athletes with competitive schedules, training commitments, or scholarship considerations. The reduced treatment duration minimizes disruption to skill development and team participation, maintaining athletic momentum during crucial developmental periods. Earlier return to activity also supports psychological well-being by reducing frustration and anxiety associated with prolonged sports absence. Physical education participation can resume sooner, helping students meet academic requirements while managing their condition effectively. The faster recovery timeline also reduces the risk of deconditioning and muscle atrophy that may occur with prolonged activity restriction.
Supporting Healthy Growth and Physical Development
Shockwave therapy’s tissue healing properties support normal apophyseal development while managing pathological inflammatory processes. The treatment stimulates appropriate bone remodeling responses that promote healthy skeletal maturation at the tibial tuberosity. Enhanced blood flow and cellular metabolism support optimal nutrient delivery to growing tissues, facilitating normal development processes. Pain reduction allows for age-appropriate physical activity participation, which is crucial for overall musculoskeletal development and fitness maintenance. The non-invasive nature eliminates concerns about growth plate disruption or interference with normal skeletal development. These factors make shockwave therapy particularly suitable for adolescents requiring effective symptom management while preserving normal growth and development patterns.
Practical Guidance for Parents and Teens
Making informed decisions about shockwave therapy requires understanding when this treatment is most appropriate, what to expect during the treatment process, and how to optimize outcomes through complementary strategies. This practical guidance helps families navigate treatment decisions and maximize therapeutic benefits for their adolescent athletes.
When to Consider Shockwave Therapy for Persistent OSD Symptoms
Shockwave therapy consideration is appropriate when conventional treatments fail to provide adequate symptom relief after 6-8 weeks of consistent application. Persistent pain interfering with daily activities, school participation, or sleep quality indicates need for more intensive therapeutic intervention. Athletes experiencing recurrent symptom flares despite appropriate activity modification and physiotherapy may benefit from shockwave therapy’s tissue healing properties. Severe cases with significant functional limitations or prolonged sports absence warrant earlier consideration of adjunctive treatment options. The presence of palpable tibial tuberosity prominence or chronic swelling may indicate tissue changes requiring active healing stimulation. Healthcare provider assessment helps determine appropriate timing and candidacy for shockwave therapy based on individual circumstances and treatment goals.
How Many Sessions Are Typically Needed for Teens
Evidence based treatment protocols recommend a minimum of 3 treatments, each 7-10 days apart for optimal therapeutic outcomes. Generally, Osgood–Schlatter Disease shockwave treatment will resolve after four to eight sessions, depending on your condition & how long you may have suffered. Most adolescents require 4-6 treatment sessions to achieve significant symptom improvement and functional restoration. Session intervals of 5-7 days allow for tissue response and recovery between treatments while maintaining therapeutic momentum. Chronic or severe cases may require additional sessions, with treatment response guiding protocol adjustments. Some patients notice improvement after 2-3 sessions, while others require the complete protocol for optimal outcomes. Treatment response monitoring helps determine when additional sessions are beneficial versus when maintenance care might be appropriate.
Combining Shockwave with Exercise and Home Care for Best Results
Integrating shockwave therapy with comprehensive rehabilitation programs produces superior outcomes compared to standalone treatment approaches. Gentle stretching exercises focusing on quadriceps, hamstrings, and hip flexors should continue between treatment sessions to maintain flexibility gains. Progressive strengthening programs can typically begin 1-2 weeks into shockwave treatment as pain levels decrease and tolerance improves. Ice application following treatment sessions helps manage any temporary increase in symptoms and supports the healing response. Activity modification guidance helps patients gradually return to sports while avoiding symptom recurrence during the healing process. Home care education including proper warm-up techniques, activity pacing, and symptom monitoring supports long-term success and prevents future episodes.
Principaux enseignements
Shockwave therapy is a promising, evidence-based option for adolescents with Osgood-Schlatter disease who do not respond to conventional care. Research shows it provides significant pain relief, accelerates tissue healing, and enables faster return to sports with excellent safety profiles. Clinical studies, including pilot trials, report no adverse events and sustained benefits up to three months after treatment. The therapy works through pain modulation, improved blood flow, stem cell activation, and enhanced tissue repair, directly addressing the condition’s underlying mechanisms. Standard treatment protocols involve 3–6 sessions spaced 5–10 days apart, with most teens experiencing improvement within 2–4 weeks. Outcomes are optimized when shockwave therapy is combined with physiotherapy, activity modification, and home care strategies. For parents and teens, consultation with qualified providers ensures safe, individualized treatment. While first-line conservative care remains important, shockwave therapy offers an effective alternative for persistent or severe cases, helping young athletes return safely to activity.
