Introduction: The Cartilage Repair Revolution
For decades, cartilage damage has been considered one of medicine’s most challenging problems. Once thought to be irreversible, cartilage degeneration has left millions of patients facing a grim prognosis of progressive joint deterioration and eventual surgical intervention. However, emerging evidence suggests that extracorporeal shockwave therapy (ESWT) may represent a paradigm shift in regenerative medicine, offering new hope for patients with cartilage damage. Recent clinical studies have demonstrated that focused acoustic waves can stimulate the body’s natural healing mechanisms, promoting chondrocyte proliferation and extracellular matrix synthesis. This non-invasive treatment modality has shown remarkable potential in treating various cartilage pathologies, from early-stage osteoarthritis to post-traumatic chondromalacia. As we delve deeper into the science behind this revolutionary therapy, we’ll explore how shockwave treatment is transforming the landscape of cartilage repair and joint preservation.
Understanding Cartilage: The Foundation of Joint Health
To appreciate the significance of shockwave therapy in cartilage repair, we must first understand the complex structure and function of this remarkable tissue. Cartilage serves as the foundation of healthy joint function, providing smooth articulation and shock absorption during movement.
What Is Cartilage and Why Does It Matter?
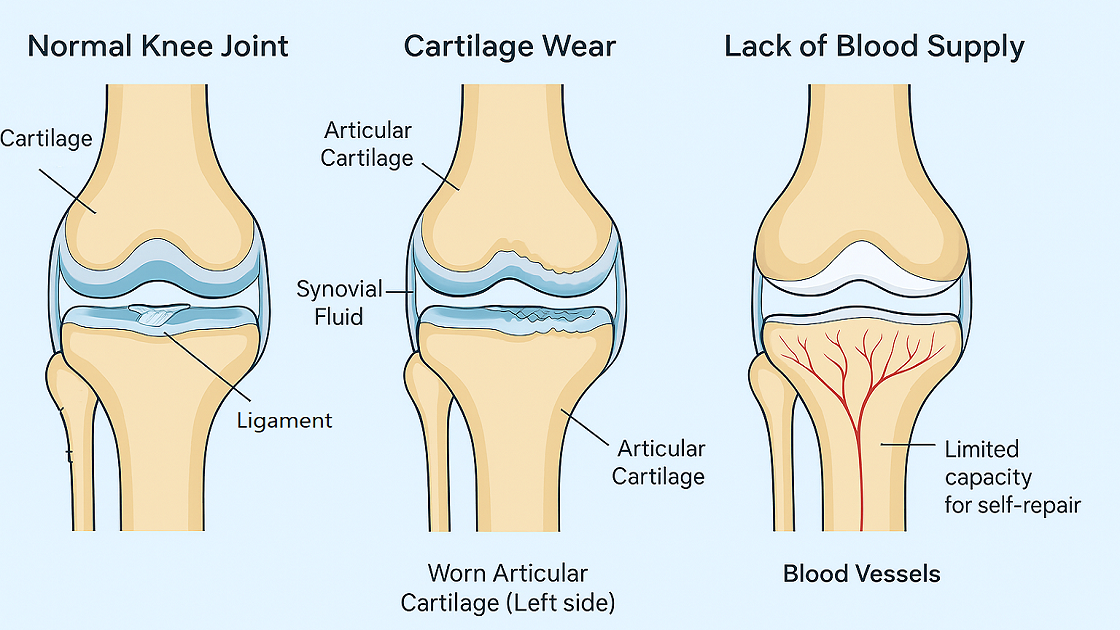
Cartilage is a specialized connective tissue composed primarily of chondrocytes embedded within an extensive extracellular matrix. This matrix consists of type II collagen fibers, proteoglycans (particularly aggrecan), and water, creating a unique viscoelastic structure. The proteoglycan-rich matrix provides compressive strength, while collagen fibers offer tensile resistance, allowing cartilage to withstand the enormous forces generated during daily activities. This remarkable tissue lacks blood vessels, lymphatics, and nerve innervation, making it metabolically dependent on synovial fluid for nutrient exchange and waste removal.
How Cartilage Damage Occurs: From Wear to Degeneration
Cartilage damage typically results from a combination of mechanical trauma, inflammatory processes, and age-related changes in cellular metabolism. Acute injuries, such as sports-related trauma or motor vehicle accidents, can cause immediate chondral defects or osteochondral fractures. Chronic overuse leads to repetitive microtrauma, gradually overwhelming the tissue’s repair capacity. Additionally, inflammatory cytokines like interleukin-1β and tumor necrosis factor-α promote matrix metalloproteinase (MMP) activation, accelerating cartilage degradation. Age-related changes in chondrocyte function, including decreased synthetic activity and increased susceptibility to apoptosis, further compromise tissue integrity.
The Challenge of Cartilage Repair: Why It’s So Difficult
The inherent challenges of cartilage repair stem from its unique biological properties and limited regenerative capacity. Unlike other tissues, cartilage lacks vascularity, preventing efficient delivery of nutrients, growth factors, and progenitor cells necessary for healing. Chondrocytes exist in a low-oxygen environment and have limited proliferative potential, particularly in mature tissue. The dense extracellular matrix impedes cell migration and tissue remodeling. Furthermore, the mechanical loading environment of joints creates additional stress on healing tissue, potentially disrupting newly formed repair tissue. These factors collectively contribute to the formation of fibrocartilage rather than hyaline cartilage, resulting in inferior biomechanical properties and increased susceptibility to future damage.
What Is Shockwave Therapy? Understanding the Technology
Shockwave therapy has emerged as a promising non-invasive treatment modality for various musculoskeletal conditions, including cartilage damage. This innovative technology harnesses the power of acoustic waves to stimulate biological healing processes at the cellular level.
What Is Extracorporeal Shockwave Therapy (ESWT) for Cartilage Repair?
Thérapie extracorporelle par ondes de choc for cartilage repair involves the application of focused acoustic waves to damaged joint tissues using specialized equipment. These high-energy acoustic pulses are generated externally and transmitted through the skin to target specific areas of cartilage pathology. The therapy utilizes either focused shockwaves, which concentrate energy at a specific depth, or radial shockwaves, which disperse energy over a broader area. Treatment parameters, including energy density, frequency, and pulse duration, are carefully calibrated based on the specific condition and patient characteristics. Modern ESWT devices incorporate real-time imaging guidance to ensure precise targeting of affected cartilage areas while minimizing impact on surrounding healthy tissues.

The Science Behind Shockwave Cartilage Regeneration
The therapeutic effects of shockwave therapy on cartilage regeneration involve complex biophysical and biochemical mechanisms that work synergistically to promote tissue healing. Understanding these mechanisms is crucial for optimizing treatment protocols and patient outcomes.
Mechanotransduction: How Mechanical Forces Trigger Healing
Mechanotransduction represents the primary mechanism by which shockwaves stimulate cartilage repair. When acoustic waves propagate through tissue, they create mechanical stress that activates mechanosensitive ion channels and integrin-mediated signaling pathways in chondrocytes. This mechanical stimulation triggers intracellular cascades involving calcium influx, activation of protein kinases, and modulation of gene expression. The Wnt/β-catenin signaling pathway, crucial for chondrocyte differentiation and matrix synthesis, becomes upregulated following shockwave treatment. Additionally, mechanotransduction enhances the expression of anabolic factors such as transforming growth factor-β and insulin-like growth factor-1, promoting proteoglycan synthesis and collagen production.
Cavitation Effects and Cellular Response
Cavitation phenomena occur when shockwaves create microscopic bubbles within the tissue matrix, followed by their rapid collapse. This process generates localized mechanical forces and microstreaming effects that enhance cellular permeability and stimulate metabolic activity. The cavitation-induced mechanical stress activates heat shock proteins, which protect chondrocytes from apoptosis and enhance their synthetic capacity. Furthermore, cavitation effects promote the release of adenosine triphosphate (ATP), which acts as an extracellular signaling molecule, stimulating purinergic receptors and initiating regenerative cascades. These effects collectively contribute to increased chondrocyte proliferation, enhanced matrix synthesis, and improved tissue integration at the repair site.
Acoustic Wave Propagation Through Joint Tissues
The propagation of acoustic waves through joint tissues involves complex interactions with different tissue types, each with distinct acoustic properties. Shockwaves travel through skin, subcutaneous tissue, muscle, and synovium before reaching cartilage, with energy attenuation occurring at each interface. The acoustic impedance mismatch between tissues creates reflection and refraction effects that influence wave intensity and distribution. Cartilage’s high water content and proteoglycan composition create unique acoustic properties that affect wave propagation patterns. Understanding these physical principles is essential for optimizing treatment parameters and ensuring adequate energy delivery to target tissues while minimizing unwanted side effects in surrounding structures.
How Shockwave Therapy Repairs Cartilage Naturally
The regenerative effects of shockwave therapy on cartilage tissue involve multiple interconnected biological processes that work together to restore joint function and reduce pain. These mechanisms represent the body’s natural healing response, enhanced and accelerated by targeted acoustic stimulation.
Cellular Mechanisms of Cartilage Regeneration
Shockwave therapy stimulates cartilage regeneration through direct effects on chondrocyte biology and behavior. The acoustic energy enhances cellular proliferation by activating cyclin-dependent kinases and promoting progression through the cell cycle. Treated chondrocytes exhibit increased metabolic activity, evidenced by enhanced glucose uptake, ATP production, and protein synthesis. The therapy also stimulates the expression of transcription factors such as SOX9, which is essential for chondrocyte differentiation and maintenance of the cartilaginous phenotype. Additionally, shockwave treatment promotes the recruitment and activation of mesenchymal stem cells from the subchondral bone and synovium, providing additional cellular resources for tissue repair and regeneration.
Growth Factor Activation and Protein Synthesis
The therapeutic effects of shockwave therapy are mediated through the activation of numerous growth factors and signaling molecules critical for cartilage repair. Treatment enhances the expression of transforming growth factor-β (TGF-β), which promotes chondrocyte proliferation and extracellular matrix synthesis. Bone morphogenetic proteins (BMPs), particularly BMP-2 and BMP-7, are upregulated following shockwave treatment, stimulating chondrogenesis and cartilage matrix formation. The therapy also increases the production of insulin-like growth factor-1 (IGF-1), which enhances protein synthesis and inhibits cartilage degradation. Furthermore, shockwave treatment modulates the expression of matrix metalloproteinases (MMPs) and their inhibitors (TIMPs), creating a favorable balance for matrix preservation and remodeling.
Subchondral Bone Healing and Cartilage Support
The relationship between subchondral bone and cartilage health is crucial for successful joint repair, and shockwave therapy addresses both components simultaneously. The treatment stimulates osteoblast activity in the subchondral bone, promoting new bone formation and improving the mechanical support for overlying cartilage. Enhanced subchondral bone density provides better distribution of mechanical loads, reducing stress concentrations that could damage cartilage. The therapy also improves the interface between cartilage and subchondral bone, promoting better integration of repair tissue. Additionally, shockwave treatment enhances the formation of new blood vessels in the subchondral region, improving nutrient delivery to the cartilage-bone interface and supporting the metabolic demands of healing tissue.
Anti-Inflammatory Effects and Pain Reduction
Shockwave therapy exerts significant anti-inflammatory effects that contribute to both symptomatic relief and tissue healing. The treatment reduces the expression of pro-inflammatory cytokines such as interleukin-1β, tumor necrosis factor-α, and interleukin-6, which are key mediators of cartilage destruction. Simultaneously, it enhances the production of anti-inflammatory molecules including interleukin-10 and transforming growth factor-β. The therapy also modulates the activity of nuclear factor-κB (NF-κB), a central regulator of inflammatory gene expression. Pain reduction occurs through multiple mechanisms, including the modulation of nociceptive pathways, reduction of inflammatory mediators, and improved tissue mechanics. The gate control theory of pain may also contribute to analgesic effects through the activation of large-diameter sensory fibers during treatment.
Cartilage Conditions Treated with Shockwave Therapy
Shockwave therapy has demonstrated clinical efficacy in treating various cartilage-related conditions across different joints. The versatility of this treatment modality makes it applicable to numerous pathologies affecting cartilage integrity and joint function.
Knee Cartilage Damage and Osteoarthritis
Knee osteoarthritis represents one of the most common applications of shockwave therapy for cartilage repair. The treatment is particularly effective for early to moderate-stage osteoarthritis, where significant cartilage architecture remains intact. Clinical studies have shown that shockwave therapy can reduce pain, improve joint function, and slow disease progression in patients with knee osteoarthritis. The therapy is also beneficial for treating focal cartilage defects, such as those resulting from sports injuries or trauma. Treatment protocols typically involve multiple sessions targeting different compartments of the knee joint, with energy parameters adjusted based on the severity of cartilage damage. Patient selection is crucial, as individuals with advanced osteoarthritis may have limited regenerative capacity.
Hip Cartilage Degeneration and Labral Tears
Hip cartilage pathology, including early-stage osteoarthritis and labral tears, responds favorably to shockwave therapy. The treatment is particularly beneficial for patients with femoroacetabular impingement (FAI) who have developed secondary cartilage damage. Shockwave therapy can help preserve remaining cartilage while addressing associated soft tissue pathology. The deep location of hip cartilage requires focused shockwave devices with sufficient penetration depth to reach target tissues effectively. Treatment success depends on accurate patient selection, with younger patients and those with localized cartilage defects showing better outcomes. The therapy can also be combined with other conservative treatments, such as physical therapy and activity modification, to optimize results.
Shoulder Cartilage Problems
Shoulder cartilage pathology, including glenohumeral osteoarthritis and glenoid labral tears, can benefit from shockwave therapy. The treatment is particularly useful for patients with early-stage arthrite who wish to avoid or delay surgical intervention. Shockwave therapy can address both the cartilage damage and associated soft tissue pathology, providing comprehensive treatment for shoulder dysfunction. The complex anatomy of the shoulder joint requires careful treatment planning to ensure adequate energy delivery to target tissues while avoiding sensitive structures. Treatment protocols may need modification based on patient positioning and joint accessibility. The therapy can be particularly beneficial for overhead athletes with cartilage damage, as it allows for continued sport participation during treatment.
Ankle and Foot Cartilage Repair
Ankle cartilage damage, including osteochondral lesions of the talus and ankle osteoarthritis, responds well to shockwave therapy. The treatment is especially effective for small to medium-sized osteochondral defects that have failed conservative management. Shockwave therapy can stimulate healing of both the cartilage and underlying bone components of osteochondral lesions. The superficial location of ankle cartilage makes it easily accessible for treatment, allowing for precise energy delivery. Treatment success rates are generally high for ankle cartilage pathology, with many patients experiencing significant pain reduction and functional improvement. The therapy can also be used as an adjunct to surgical treatments, such as microfracture or autologous chondrocyte implantation, to enhance healing outcomes.
Recovery Timeline: What to Expect After Cartilage Shockwave Therapy
Understanding the recovery timeline following shockwave therapy for cartilage repair helps patients set realistic expectations and optimize their treatment outcomes. The healing process occurs in distinct phases, each characterized by specific biological events and clinical milestones.
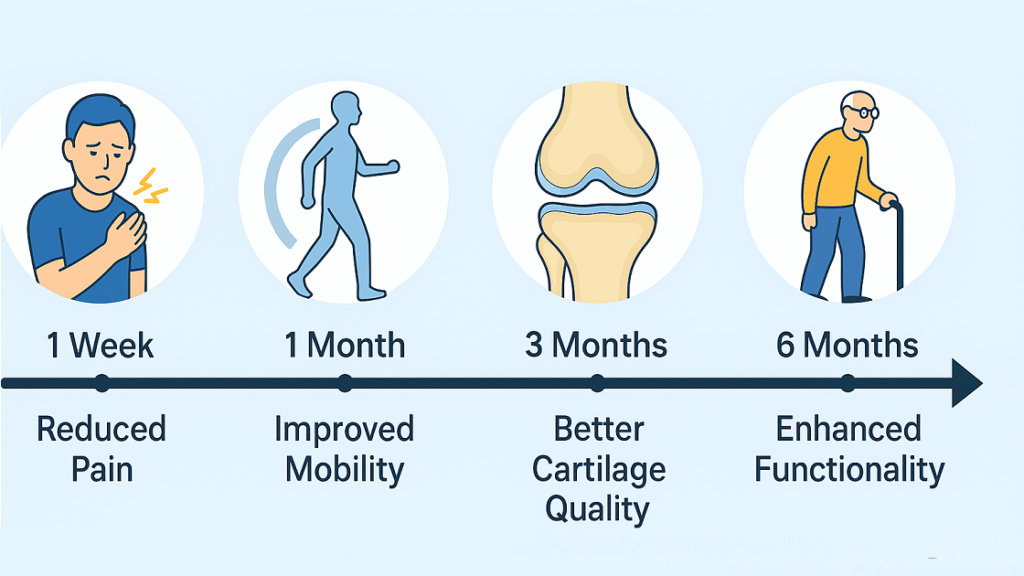
Immediate Post-Treatment Response
The immediate post-treatment period, spanning the first 24-48 hours following shockwave therapy, is characterized by the initiation of biological healing processes. Patients may experience mild to moderate discomfort at the treatment site, which typically resolves within 24-48 hours. This discomfort reflects the normal inflammatory response to mechanical stimulation and indicates that the therapy is activating cellular repair mechanisms. Some patients may notice temporary swelling or erythema at the treatment site, which is a normal response to the acoustic energy. During this period, patients should avoid anti-inflammatory medications that could interfere with the healing process. Light activities are generally permitted, but high-impact exercises should be avoided to prevent disruption of the initial healing response.
Short-Term Recovery (1-4 Weeks)
The short-term recovery phase is marked by the onset of cellular proliferation and early matrix synthesis. Patients may begin to notice subtle improvements in pain levels and joint stiffness during this period. The inflammatory response typically subsides, and any post-treatment discomfort should resolve completely. Cellular activity increases significantly during this phase, with enhanced chondrocyte proliferation and growth factor expression. Patients should gradually increase their activity levels while avoiding excessive loading of the treated joint. Physical therapy may be initiated during this period to optimize joint mobility and muscle strength. Some patients may experience fluctuations in symptoms as the healing process progresses, which is considered normal. Regular follow-up appointments allow for monitoring of progress and adjustment of treatment protocols if necessary.
Medium-Term Results (1-3 Months)
The medium-term recovery period represents a critical phase where significant tissue remodeling and functional improvements typically occur. Patients often experience substantial pain reduction and improved joint function during this timeframe. Extracellular matrix synthesis becomes more organized, with enhanced collagen and proteoglycan production. The subchondral bone healing process contributes to improved mechanical support for the overlying cartilage. Patients can typically return to most normal activities during this period, with gradual progression to higher-impact exercises as tolerated. Advanced imaging studies may show early signs of cartilage repair and improved tissue quality. The full anti-inflammatory effects of the therapy become apparent, with reduced joint swelling and improved range of motion. This period is crucial for optimizing long-term outcomes through appropriate rehabilitation and activity modification.
Long-Term Outcomes (3-12 Months and Beyond)
Long-term outcomes following shockwave therapy for cartilage repair continue to improve over 6-12 months as tissue maturation progresses. The newly formed cartilage-like tissue undergoes continued remodeling and integration with surrounding healthy cartilage. Patients typically experience sustained pain relief and functional improvement that can persist for years following treatment. The structural integrity of the repair tissue continues to strengthen through appropriate mechanical loading and ongoing cellular activity. Long-term follow-up studies demonstrate that many patients maintain their functional gains and avoid progression to more advanced joint degeneration. However, individual outcomes vary based on factors such as age, initial severity of damage, and compliance with post-treatment recommendations. Some patients may benefit from periodic booster treatments to maintain optimal results, particularly those with ongoing mechanical stresses or predisposing factors for cartilage degeneration.
Expert Opinions: What Medical Professionals Say
The medical community’s perspective on shockwave therapy for cartilage repair continues to evolve as more clinical evidence becomes available. Leading specialists across various disciplines have shared their insights on this emerging treatment modality.
Orthopedic Surgeons’ Perspectives
Orthopedic surgeons have increasingly recognized shockwave therapy as a valuable non-surgical option for cartilage repair. Many specialists view it as an important bridge treatment that can delay or potentially eliminate the need for more invasive procedures. Leading orthopedic surgeons emphasize the importance of proper patient selection, noting that early-stage cartilage damage responds more favorably than advanced degenerative changes. The treatment is particularly valued for its ability to address both cartilage and subchondral bone pathology simultaneously. Surgeons also appreciate the minimal downtime associated with the therapy, allowing patients to maintain their daily activities while undergoing treatment. However, they stress the importance of realistic expectations and the need for comprehensive evaluation to determine the most appropriate treatment approach for each individual patient.
Rheumatologists’ Clinical Experience
Rheumatologists have observed promising results with shockwave therapy in their patients with inflammatory arthritis and osteoarthritis. They particularly value the anti-inflammatory effects of the treatment, which complement traditional pharmacological interventions. Many rheumatologists report that shockwave therapy can reduce the need for intra-articular corticosteroid injections and may help preserve joint function in patients with early-stage disease. The therapy’s ability to modulate inflammatory pathways at the cellular level aligns well with current understanding of arthritis pathophysiology. Rheumatologists emphasize the importance of integrating shockwave therapy into comprehensive treatment plans that include appropriate medications, physical therapy, and lifestyle modifications. They also note that the treatment can be particularly beneficial for patients who cannot tolerate or prefer to avoid systemic medications.
Sports Medicine Specialists’ Insights
Sports medicine specialists have been early adopters of shockwave therapy for cartilage repair, particularly in active individuals who wish to avoid surgical interventions. They report excellent outcomes in treating acute cartilage injuries and chronic overuse conditions in athletes. The therapy’s ability to promote healing while allowing continued participation in sports activities is particularly valued in this population. Sports medicine physicians emphasize the importance of combining shockwave therapy with appropriate biomechanical corrections and training modifications to prevent recurrence of injury. They also note that the treatment can be particularly effective when used as part of a comprehensive rehabilitation program that addresses underlying movement patterns and muscle imbalances. Many specialists report that athletes treated with shockwave therapy demonstrate faster return to sport and reduced risk of future cartilage damage.
Shockwave Therapy for Cartilage: FAQs and Patient Concerns
Shockwave therapy does more than mask pain—it stimulates biological processes like growth factor release and mechanotransduction, helping your body actively repair and regenerate damaged cartilage.
While the knee is a common target, shockwave therapy is also effective for hip, shoulder, and ankle cartilage issues, offering joint-specific benefits across the body.
It works best for early- to mid-stage cartilage degeneration, helping patients avoid or delay surgery while restoring joint mobility and comfort.
Most patients see gradual improvements over 3–6 months, and studies show many enjoy long-term benefits for years with proper joint care.
From orthopedic surgeons to sports medicine specialists, many professionals recommend shockwave therapy as a safe, non-surgical, and research-supported option.
Principaux enseignements
Shockwave therapy is a major advancement in traitement non chirurgical for cartilage damage, offering hope to patients with joint issues. It promotes natural cartilage repair through mechanisms like mechanotransduction, growth factor activation, and anti-inflammatory effects. Studies show it effectively treats cartilage problems in the knee, hip, shoulder, and ankle—especially in early-stage damage. By reducing pain and preserving joint function, shockwave therapy improves quality of life and may delay or prevent surgery. Recovery is gradual, with most patients seeing progress over 3–6 months. Long-term results are promising, with many maintaining functional improvements for years. Medical experts from orthopedics to sports medicine recognize its value, highlighting shockwave therapy as a trusted, non-invasive alternative to traditional procedures.
Resources and References
- Le temps ne guérit pas toutes les blessures, mais les ondes de choc pourraient le faire
- Quels sont les effets secondaires négatifs de la thérapie par ondes de choc ?
- The effect of extracorporeal shock wave therapy on the treatment of moderate to severe knee osteoarthritis and cartilage lesion
- Mechanotransduction and cartilage integrity
- Les effets biologiques de la thérapie extracorporelle par ondes de choc (TEOC) sur le tissu tendineux