Chronic back pain affects millions of adults worldwide, creating a significant burden on healthcare systems and dramatically impacting quality of life for those who suffer from this debilitating condition. As traditional treatment approaches often fall short of providing lasting relief, innovative therapeutic modalities like extracorporeal shockwave therapy (ESWT) are emerging as promising alternatives that offer hope for patients seeking effective, non-invasive solutions to their persistent pain challenges.
Introduction
The landscape of back pain management has evolved dramatically over recent decades, with healthcare providers and patients increasingly recognizing the limitations of conventional approaches and seeking more effective, sustainable treatment options. This shift toward innovative therapeutic modalities reflects both advances in our understanding of pain physiology and the growing demand for treatments that address root causes rather than merely masking symptoms.
Understanding the Prevalence of Back Pain in Adults
Chronic low back pain represents one of the most prevalent musculoskeletal disorders globally, affecting approximately 80% of adults at some point during their lifetime. The condition imposes substantial economic burdens, with annual healthcare costs exceeding billions of dollars due to direct medical expenses and indirect costs from lost productivity. Epidemiological studies demonstrate that lumbar spine disorders account for more years lived with disability than any other condition worldwide. The prevalence increases with age, with individuals over 65 experiencing the highest rates of chronic symptomatology. Risk factors include occupational demands, sedentary lifestyles, obesity, psychological stress, and genetic predisposition. The complexity of chronic back pain etiology necessitates multifaceted treatment approaches that address both biomechanical and psychosocial contributors to persistent symptoms.
Why Non-Invasive Treatments Are Becoming Popular
The growing preference for non-invasive back pain treatments reflects increasing awareness of the limitations and risks associated with traditional interventions, particularly long-term pharmaceutical management and surgical procedures. Opioid crisis concerns have prompted both patients and providers to seek alternative pain management strategies that avoid addiction potential and systemic side effects. Non-invasive modalities offer several advantages, including reduced complication risks, shorter recovery times, preservation of anatomical structures, and compatibility with active lifestyles. Patient autonomy and treatment preference surveys consistently demonstrate strong preferences for conservative approaches when efficacy is comparable to invasive alternatives. Additionally, cost-effectiveness analyses increasingly favor non-invasive treatments due to lower procedural costs, reduced hospitalization requirements, and decreased long-term healthcare utilization patterns.
Understanding Chronic and Acute Back Pain: Causes and Impacts
The complexity of back pain syndromes requires comprehensive understanding of their underlying mechanisms, contributing factors, and far-reaching impacts on patient functioning. Distinguishing between chronic and acute presentations is essential for developing appropriate treatment strategies and establishing realistic therapeutic goals that address both immediate symptoms and long-term functional restoration.
Common Causes of Back Pain: Muscular, Skeletal, and Neurological
Mal de dos etiology encompasses diverse pathophysiological mechanisms affecting multiple anatomical structures within the lumbar spine complex. Muscular causes include myofascial pain syndrome, muscle strains, and trigger point activation resulting from biomechanical imbalances, overuse patterns, or acute trauma. Skeletal pathologies comprise degenerative disc disease, facet joint arthrite, spinal stenosis, spondylolisthesis, and vertebral compression fractures that alter normal spinal mechanics and load distribution. Neurological components involve nerve root impingement, central sensitization phenomena, and neuropathic pain mechanisms that perpetuate symptoms beyond tissue healing timelines. Inflammatory processes, including cytokine-mediated responses and autoimmune reactions, contribute to pain persistence and tissue destruction. Additionally, psychosocial factors such as stress, depression, and fear-avoidance behaviors significantly influence pain perception and treatment outcomes.
Chronic and Acute Back Pain: Differences in Treatment Approaches
Acute and chronic back pain represent distinct clinical entities requiring fundamentally different therapeutic strategies based on their underlying pathophysiology and treatment objectives. Acute back pain, typically lasting less than six weeks, primarily involves tissue damage and inflammatory responses that generally respond well to rest, anti-inflammatory medications, and activity modification. Treatment goals focus on symptom relief, preventing chronicity, and facilitating rapid return to normal function. Chronic back pain, persisting beyond three months, involves complex neuroplastic changes, central sensitization, and psychosocial factors that require comprehensive, multimodal approaches. Chronic conditions necessitate treatments that address neuroplasticity, improve function, and enhance coping strategies rather than simply reducing pain intensity. The transition from acute to chronic pain involves maladaptive changes in central nervous system processing that must be specifically targeted through specialized interventions.
How Lifestyle, Posture, and Ergonomics Influence Chronic Back Pain
Contemporary lifestyle factors significantly contribute to chronic back pain development and perpetuation through sustained postural stress, reduced physical activity, and ergonomic deficiencies in work and home environments. Prolonged sitting positions create increased intradiscal pressure, weakened postural muscles, and altered movement patterns that predispose to injury and pain development. Poor workplace ergonomics, including inadequate lumbar support, improper monitor positioning, and repetitive lifting tasks, contribute to cumulative trauma and degenerative changes over time. Sedentary lifestyles result in decreased muscle strength, reduced flexibility, and impaired proprioception that compromise spinal stability and movement efficiency. Sleep quality and positioning significantly affect spinal health, with inadequate support during rest periods contributing to morning stiffness and pain exacerbation. Addressing these modifiable risk factors represents crucial components of comprehensive back pain management strategies.
Psychological and Emotional Impacts of Persistent Back Pain
Chronic back pain creates profound psychological and emotional consequences that often exceed the impact of physical symptoms on overall quality of life and functional capacity. Depression and anxiety disorders occur at significantly higher rates among chronic pain sufferers, with bidirectional relationships between mood disorders and pain intensity. Fear-avoidance behaviors develop as protective mechanisms but ultimately contribute to physical deconditioning, social isolation, and functional decline that perpetuate disability. Sleep disturbances, including difficulty initiating sleep, frequent awakenings, and non-restorative rest, exacerbate both pain and mood symptoms while impairing healing processes. Cognitive effects, such as attention deficits and memory problems, result from pain-related brain changes and medication side effects. Social relationships suffer due to activity limitations, mood changes, and reduced participation in family and recreational activities, leading to isolation and relationship strain.
What is Shockwave Therapy for Back Pain?
Shockwave therapy represents a sophisticated technological approach to pain management that harnesses the power of acoustic energy to promote healing and pain relief at the cellular level. Understanding the fundamental principles underlying this innovative treatment modality is essential for appreciating its therapeutic potential and appropriate clinical applications in back pain management.
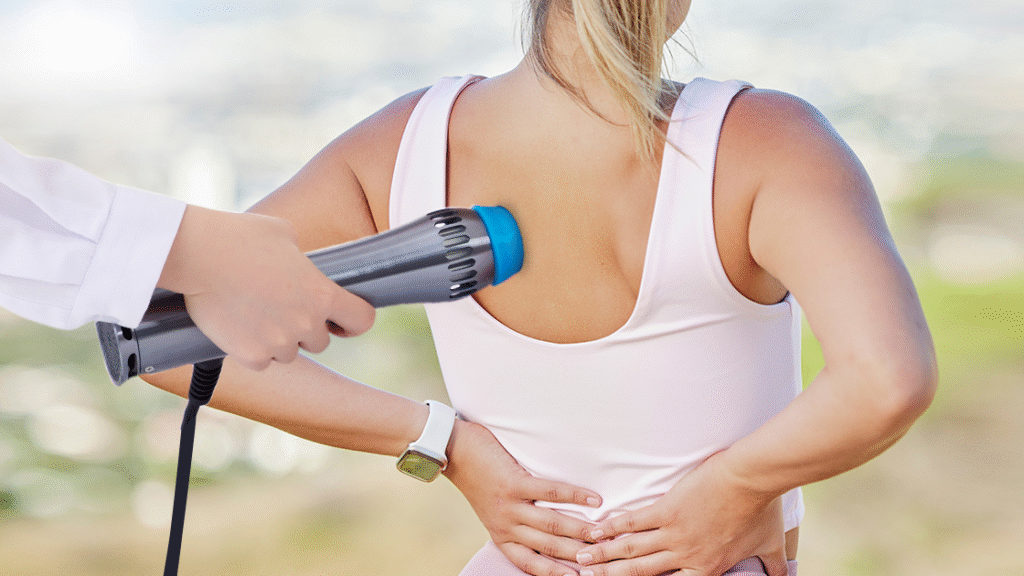
Defining Shockwave Therapy
Extracorporeal shockwave therapy (ESWT) utilizes high-energy acoustic waves generated outside the body and transmitted through skin and soft tissues to targeted treatment areas within deeper anatomical structures. The technology employs focused or radial wave delivery systems that create mechanical stress and microtrauma at the cellular level, triggering beneficial biological responses. Focused shockwaves concentrate energy at specific depths and locations, providing precise treatment targeting for deep tissue pathologies. Radial shockwaves disperse energy over broader areas, making them suitable for superficial tissue treatment and trigger point therapy. Treatment parameters including energy level, pulse frequency, and total number of shocks are customized based on individual patient needs and specific pathological conditions. The non-invasive nature eliminates risks associated with surgical procedures while providing measurable therapeutic benefits for various musculoskeletal conditions.
Mechanism of Action: How Acoustic Waves Promote Tissue Healing
Shockwave therapy promotes tissue healing through multiple interconnected biological mechanisms that address both acute inflammatory processes and chronic degenerative changes. Mechanical stimulation from acoustic waves triggers neovascularization through upregulation of angiogenic growth factors, improving local blood flow and nutrient delivery to healing tissues. Cavitation effects create microscopic bubbles that collapse and generate secondary shock waves, enhancing cellular permeability and facilitating metabolic processes. Nitric oxide release promotes vasodilation and anti-inflammatory responses while stimulating tissue repair mechanisms. Substance P depletion reduces pain transmission through C-fiber pathways, providing direct analgesic effects. Collagen synthesis enhancement improves tissue strength and structural integrity in damaged areas. Additionally, stem cell activation and recruitment accelerate tissue regeneration processes, contributing to long-term healing and functional restoration.
Advantages of Shockwave Therapy Compared to Conventional Back Pain Treatments
Shockwave therapy offers significant advantages over conventional back pain treatments, making it an attractive option for patients seeking effective, low-risk alternatives to traditional interventions. The non-invasive nature eliminates surgical risks, anesthesia requirements, and extended recovery periods associated with invasive procedures. Unlike pharmaceutical approaches, shockwave therapy provides localized treatment effects without systemic side effects or drug interaction concerns. Treatment sessions are typically brief, lasting 10-15 minutes, making them convenient for busy schedules and reducing healthcare facility burden. The therapy addresses underlying pathophysiology rather than simply masking symptoms, potentially providing longer-lasting relief compared to symptomatic treatments. Cost-effectiveness analyses demonstrate favorable outcomes when compared to long-term medication management or surgical interventions. Additionally, shockwave therapy can be combined with other conservative treatments to enhance overall therapeutic outcomes while maintaining its excellent safety profile.
How Shockwave Therapy Targets Chronic Back Pain
The application of shockwave therapy to chronic back pain represents a targeted approach that addresses the complex pathophysiological mechanisms underlying persistent spinal disorders. By understanding how acoustic waves interact with various tissue types and pain processes, clinicians can optimize treatment protocols to achieve maximum therapeutic benefit for their patients.
Targeting Chronic Muscle and Ligament Pain
Shockwave therapy effectively addresses chronic muscle and ligament pain through direct mechanical effects and secondary biological responses that promote healing and pain reduction. Recent systematic reviews and meta-analyses demonstrate that all treated patients had significantly reduced pain and improved functional impairment immediately after procedures and one month later. The acoustic waves target myofascial trigger points, disrupting pathological muscle contractions and reducing local inflammation. Ligamentous structures benefit from enhanced collagen synthesis and improved tissue organization following treatment. Muscle spasm reduction occurs through neurological mechanisms that interrupt pathological reflex patterns contributing to chronic tension. The therapy promotes muscle fiber regeneration and reduces scar tissue formation in previously injured areas. Treatment of paraspinal muscles improves spinal stability and movement patterns, addressing biomechanical contributors to ongoing pain. Multiple treatment sessions allow for progressive tissue remodeling and sustained pain relief.
Promoting Spinal Tissue Regeneration and Reducing Inflammation
Shockwave therapy’s regenerative effects on spinal tissues represent a fundamental advantage in treating chronic back pain conditions characterized by degenerative changes and persistent inflammation. The treatment stimulates osteoblast activity and bone remodeling processes, potentially improving vertebral integrity and facet joint function. Intervertebral disc nutrition enhancement occurs through improved diffusion processes and reduced inflammatory mediators that inhibit disc metabolism. Anti-inflammatory effects result from modulation of cytokine production and reduction of pro-inflammatory substances in affected tissues. Neovascularization promotion increases blood supply to poorly vascularized spinal structures, supporting healing and metabolic function. The therapy addresses chronic inflammatory cascades that perpetuate pain and tissue destruction, breaking cycles of ongoing damage. Growth factor upregulation facilitates tissue repair and regeneration processes essential for long-term recovery and functional restoration.
Pain Relief Without Surgery or Pharmaceuticals
The ability of shockwave therapy to provide significant pain relief without surgical intervention or long-term pharmaceutical dependence represents a major advantage for chronic back pain sufferers. Research demonstrates that ESWT in chronic low back pain patients results in significant and quantifiable reductions in pain and disability in the short term. Neurological mechanisms include substance P depletion, which reduces pain signal transmission through peripheral and central pathways. Gate control theory activation occurs through large-diameter nerve fiber stimulation that inhibits pain transmission at spinal cord levels. Endorphin release provides natural analgesic effects without external medication administration. The treatment addresses neuropathic pain components through nerve desensitization and reduced central sensitization phenomena. Long-term pain relief results from tissue healing and regeneration rather than temporary symptom masking. Patients can maintain active lifestyles during treatment without activity restrictions or recovery periods associated with invasive procedures.
Who Can Benefit Most from Shockwave Therapy
Optimal candidates for shockwave therapy include patients with specific chronic back pain characteristics that align with the treatment’s mechanisms of action and demonstrated efficacy. Individuals with myofascial pain syndrome, particularly those with identifiable trigger points and muscle tension patterns, respond favorably to radial shockwave applications. Patients with degenerative disc disease or facet joint arthritis may benefit from focused shockwave therapy targeting deeper spinal structures. Chronic pain sufferers who have failed conservative treatments but wish to avoid surgical interventions represent ideal candidates for this approach. Athletes and active individuals with chronic back pain benefit from the therapy’s ability to promote healing while allowing continued activity participation. Patients seeking non-pharmaceutical pain management due to medication intolerance or addiction concerns find shockwave therapy particularly valuable. Additionally, individuals with chronic pain accompanied by functional limitations may experience improvements in both pain and disability measures.
Treatment Protocols and What to Expect
Understanding the practical aspects of shockwave therapy treatment helps patients prepare appropriately and maintain realistic expectations throughout their therapeutic journey. Comprehensive knowledge of treatment protocols, session experiences, and recovery timelines enables informed decision-making and optimal treatment outcomes.
Duration, Frequency, and Typical Number of Sessions
Shockwave therapy treatment protocols vary based on individual patient needs, specific pathology characteristics, and treatment response patterns observed during therapy progression. Individual treatment sessions typically last 10-15 minutes, with actual shockwave application comprising 5-10 minutes of the total appointment time. Treatment frequency commonly ranges from once weekly to twice weekly, depending on condition severity and patient tolerance levels. Most patients require 3-6 treatment sessions to achieve optimal therapeutic outcomes, though some chronic conditions may benefit from additional sessions. Session intervals of 5-7 days allow for tissue recovery and biological responses to develop between treatments. Treatment intensity typically increases gradually, starting with lower energy levels and progressing based on patient response and tolerance. Follow-up sessions may be scheduled 3-6 months after initial treatment completion to maintain therapeutic benefits and address any symptom recurrence.
Sensations During Therapy and Possible Side Effects
Patients undergoing shockwave therapy experience various sensations during treatment that are generally well-tolerated and indicate appropriate therapeutic energy delivery to target tissues. Common sensations include mild to moderate discomfort, pulsing, or pressure sensations at treatment sites that typically subside immediately after session completion. Some patients describe tingling or numbness in treated areas that resolves within minutes of treatment cessation. Energy level adjustments during treatment allow for comfort optimization while maintaining therapeutic efficacy. Post-treatment side effects are typically mild and transient, including temporary soreness, slight swelling, or skin redness at application sites. Rare adverse effects may include bruising or temporary nerve irritation that resolves spontaneously within days. Most patients can resume normal activities immediately following treatment sessions. Pre-treatment analgesics are occasionally recommended for patients with high pain sensitivity or anxiety about treatment discomfort.
Combining Shockwave Therapy with Physiotherapy and Orthobiologics
Integrative treatment approaches combining shockwave therapy with complementary modalities often produce superior outcomes compared to single-treatment protocols. Physiotherapy integration enhances outcomes through movement pattern correction, strength training, and flexibility improvement that address biomechanical contributors to chronic pain. Exercise prescription following shockwave sessions optimizes tissue healing through controlled loading and improved circulation. Manual therapy techniques, including mobilization and soft tissue treatments, complement shockwave effects through synergistic mechanisms. Orthobiologic treatments such as platelet-rich plasma or stem cell therapy may enhance tissue regeneration when combined with shockwave stimulation. Anti-inflammatory modalities including cold therapy or electrical stimulation can manage post-treatment discomfort while supporting healing processes. Patient education regarding activity modification and self-management strategies maximizes treatment benefits and prevents symptom recurrence.
Recovery Timeline and Expected Outcomes
Understanding realistic recovery timelines and expected outcomes helps patients maintain appropriate expectations and commitment to treatment protocols throughout their therapeutic journey. Initial pain relief may occur within 24-48 hours following first treatment sessions, though some patients require multiple sessions before experiencing significant improvement. Progressive pain reduction typically occurs over 2-4 weeks, with maximum benefits often realized 6-12 weeks after treatment completion. Functional improvements, including increased mobility and activity tolerance, generally parallel pain reduction timelines but may continue improving for several months. Clinical studies reveal that treated patients had significantly reduced pain and improved functional impairment immediately after procedures and 1 month later. Individual response variations depend on factors including condition chronicity, overall health status, and adherence to complementary treatment recommendations. Long-term outcome studies suggest sustained benefits lasting 6-12 months or longer in many patients, with some requiring periodic maintenance treatments for optimal symptom control.
Clinical Evidence and Effectiveness
The scientific foundation supporting shockwave therapy for chronic back pain continues to expand through rigorous research methodologies and well-designed clinical studies. Understanding the current evidence base provides essential context for treatment decisions and helps establish realistic expectations for therapeutic outcomes.
Research Studies on Shockwave Therapy for Back Pain Relief
Multiple systematic reviews and meta-analyses have examined shockwave therapy efficacy for chronic low back pain, providing robust evidence supporting its therapeutic value. A comprehensive meta-analysis of 632 patients was conducted to analyze and determine the efficacy and safety of ESWT for chronic low back pain. Randomized controlled trials consistently demonstrate significant pain reduction and functional improvement compared to control groups receiving sham treatments or standard care. Current research shows that ESWT can be used for pain relief, though studies examining effects on chronic low back pain, balance ability, and depression remain limited. Comparative studies indicate that both focused and radial shockwave modalities produce beneficial outcomes, though optimal treatment parameters continue to be refined through ongoing research. Long-term follow-up studies demonstrate sustained benefits extending 6-12 months post-treatment, suggesting lasting therapeutic effects rather than temporary symptom relief.
Success Rates in Chronic vs. Acute Conditions
Clinical research reveals differential success rates between chronic and acute back pain conditions, with specific patterns emerging from large-scale studies and meta-analyses. Chronic low back pain conditions demonstrate success rates ranging from 70-85% for significant pain reduction and functional improvement measures. Acute back pain episodes show somewhat higher response rates, typically achieving 85-95% success in pain resolution and return to normal function. Results showed that the shockwave group saw high improvements in pain intensity and balance ability compared to traditional physical therapy groups. Treatment response appears inversely related to symptom duration, with patients suffering from chronic pain for shorter periods generally achieving better outcomes. Success criteria variations across studies include different pain reduction thresholds and functional outcome measures, making direct comparisons challenging. However, consistent patterns emerge showing clinically meaningful improvements in pain, function, and quality of life measures across diverse patient populations.
Long-Term Benefits and Sustainability of Results
Long-term outcome studies provide crucial insights into the sustainability of shockwave therapy benefits and the need for maintenance treatments in chronic back pain management. Follow-up periods extending 12-24 months demonstrate maintained pain reduction and functional improvements in the majority of successfully treated patients. Factors influencing long-term success include initial treatment response magnitude, adherence to post-treatment exercise recommendations, and lifestyle modification implementation. Some patients experience gradual symptom recurrence requiring periodic maintenance treatments, typically at 6-12 month intervals to sustain optimal outcomes. Combined treatment approaches incorporating ongoing exercise therapy and ergonomic modifications show superior long-term results compared to shockwave therapy alone. Patient satisfaction surveys consistently indicate high levels of treatment satisfaction and willingness to recommend the therapy to others with similar conditions. Cost-effectiveness analyses support long-term value when considering reduced medication use, decreased healthcare utilization, and improved work productivity.
Integrating Shockwave Therapy into Holistic Back Care
Optimal outcomes with shockwave therapy require integration into comprehensive back care programs that address multiple contributors to chronic pain and promote long-term spinal health. This holistic approach recognizes the complex, multifactorial nature of chronic back pain and the importance of lifestyle modifications in maintaining treatment benefits.
Exercise and Stretching Routines to Support Healing
Structured exercise programs complement shockwave therapy by addressing biomechanical factors that contribute to chronic back pain while promoting tissue healing and functional restoration. Core strengthening exercises targeting deep stabilizing muscles improve spinal stability and reduce mechanical stress on healing tissues. Flexibility programs focusing on hip flexors, hamstrings, and thoracic spine mobility address common movement restrictions that perpetuate back pain patterns. Graduated aerobic conditioning promotes cardiovascular health and endurance while supporting tissue healing through improved circulation and nutrient delivery. Movement pattern training corrects faulty biomechanics that contribute to ongoing tissue stress and pain perpetuation. Proprioceptive and balance training address neuromuscular control deficits common in chronic pain patients. Post-treatment exercise timing should allow for initial tissue response to shockwave therapy while promoting beneficial loading for optimal healing outcomes.
Lifestyle Adjustments for Long-Term Back Health
Comprehensive lifestyle modifications represent essential components of successful long-term back pain management and prevention of symptom recurrence following shockwave therapy. Ergonomic assessments and workplace modifications reduce occupational risk factors that contribute to ongoing spinal stress and tissue irritation. Sleep hygiene optimization, including appropriate mattress selection and sleeping positions, supports tissue healing and reduces morning pain and stiffness. Weight management strategies address obesity-related factors that increase spinal loading and contribute to degenerative changes over time. Stress management techniques including relaxation training and mindfulness practices help modulate pain perception and reduce muscle tension patterns. Activity modification strategies promote safe participation in recreational and occupational activities while avoiding movements or positions that exacerbate symptoms. Regular movement breaks during prolonged sitting or static positions prevent tissue stiffness and promote spinal health maintenance.
Nutrition and Anti-Inflammatory Support
Nutritional strategies play crucial roles in supporting tissue healing following shockwave therapy while addressing systemic inflammation that contributes to chronic pain conditions. Anti-inflammatory dietary patterns emphasizing omega-3 fatty acids, antioxidants, and phytonutrients support tissue repair while reducing inflammatory burden. Adequate protein intake provides essential amino acids for collagen synthesis and tissue regeneration processes activated by shockwave treatment. Hydration maintenance supports tissue metabolism and waste product removal essential for optimal healing responses. Specific nutrients including vitamin D, magnesium, and B-complex vitamins support nerve function and muscle metabolism. Elimination of pro-inflammatory foods including processed sugars, trans fats, and excessive omega-6 fatty acids reduces systemic inflammation contributing to chronic pain. Supplemental anti-inflammatory compounds such as turmeric, boswellia, and fish oil may provide additional support for pain management and tissue healing processes.
Key Takeaways: Is Shockwave Therapy Right for Your Back Pain?
Shockwave therapy offers an effective, non-invasive option for chronic back pain, especially for those unsatisfied with conventional treatments or seeking to avoid surgery. Clinical evidence supports its ability to reduce pain, improve function, and target underlying muscle, ligament, and degenerative issues rather than just masking symptoms. Ideal candidates include patients with chronic muscle or ligament pain, degenerative conditions, or those seeking non-pharmaceutical pain management. Minimal side effects, brief sessions, and compatibility with busy lifestyles make it convenient for many individuals. Optimal results depend on proper candidate selection, realistic expectations, and integration with complementary therapies such as exercise, ergonomics, and lifestyle adjustments. Maintenance sessions may be needed for lasting benefits. When combined with a comprehensive back care program addressing biomechanical, psychosocial, and lifestyle factors, shockwave therapy can provide significant, sustained relief for those who have exhausted conservative options and wish to avoid long-term medication or surgery.
Références et lectures complémentaires
- Douleur chronique ? Il est peut-être temps d'essayer les ondes de choc
- The Power of Shockwave Therapy for Pain Management
- Epidemiology of chronic low back pain in US adults: National Health and Nutrition Examination Survey 2009–2010
- Extracorporeal Shock Wave Therapy in Musculoskeletal Disorders: A Review
- Effets de la thérapie extracorporelle par ondes de choc sur les patients souffrant de lombalgie chronique et sur leur capacité d'équilibre dynamique
Efficacité et sécurité de la thérapie extracorporelle par ondes de choc dans la lombalgie chronique : revue systématique et méta-analyse de 632 patients
