Introduction
Chronic wounds are wounds that fail to progress through the normal physiological stages of healing within an expected timeframe, often persisting for weeks or months despite appropriate clinical management. These wounds commonly include diabetic foot ulcers, pressure ulcers, vascular ulcers, and post-surgical wounds with delayed closure.Their prolonged nature typically involves impaired microcirculation, persistent inflammation, cellular senescence, and reduced regenerative signaling, all of which disrupt normal tissue repair. As traditional wound care strategies alone are sometimes insufficient, increasing attention has turned toward non-invasive physical therapies that can biologically stimulate healing processes. Shockwave therapy has emerged as a promising adjunctive modality, capable of mechanically activating angiogenesis, tissue regeneration, and inflammatory modulation. When considered alongside other biophysical approaches such as laser therapy, shockwave therapy represents an evolving and evidence-informed strategy in comprehensive chronic wound management.
1. Chronic Wounds: Types and Therapeutic Challenges
1.1 What Are Chronic Wounds?
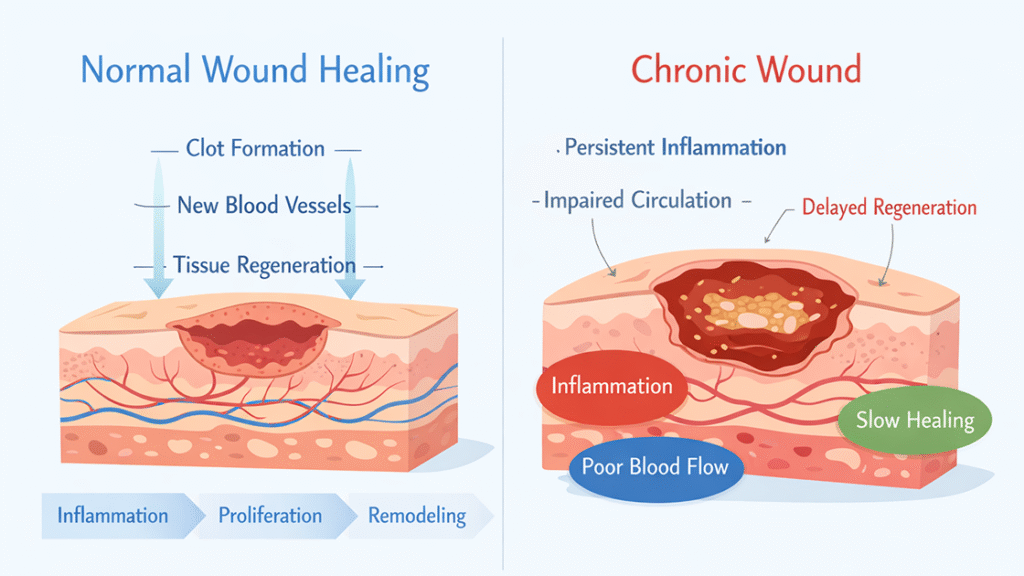
The defining feature of chronic wounds is a stalled or disordered progression through the normal stages of wound healing—hemostasis, inflammation, proliferation, and remodeling. Unlike acute wounds, which typically resolve within weeks, chronic wounds remain trapped in a pathological inflammatory state. This prolonged inflammation leads to excessive protease activity, degradation of growth factors, and impaired extracellular matrix formation. Fibroblast dysfunction and cellular senescence further compromise the regenerative capacity of the tissue.
From a clinical perspective, chronic wounds often present with persistent exudate, fragile granulation tissue, and delayed epithelialization; they may also demonstrate a tendency for recurrent breakdown. These pathological features reflect underlying molecular imbalances that conventional wound care alone may struggle to correct, necessitating adjunctive therapies capable of reactivating stalled biological processes.
1.2 Common Types of Chronic Wounds
Although chronic wounds arise from diverse etiologies, they share overlapping pathophysiological features. Diabetic foot ulcers primarily stem from neuropathy, microvascular disease, and metabolic dysregulation, which together result in impaired sensation and ischemia. Pressure ulcers develop due to sustained mechanical compression, leading to compromised blood flow and tissue hypoxia, particularly in immobile individuals. Venous leg ulcers are typically associated with venous hypertension and chronic edema, whereas arterial ulcers are caused by insufficient arterial perfusion.
Post-surgical wounds may also become chronic when tissue perfusion is compromised or mechanical stress disrupts healing. Despite differing origins, all chronic wound types exhibit reduced angiogenesis, altered immune responses, and diminished cellular activity, making them suitable targets for regenerative stimulation.
1.3 Limitations of Traditional Therapies
Standard wound care focuses on debridement, moisture balance, infection control, pressure offloading, and management of systemic conditions. While these measures are essential, they do not directly address the cellular and molecular dysfunctions that characterize chronic wounds. Reduced blood supply, impaired signaling pathways, and persistent inflammation often remain uncorrected.
Advanced treatments such as skin substitutes or surgical interventions may offer benefits but carry higher costs and risks. Consequently, there is growing interest in therapies that can non-invasively enhance the wound’s biological environment, complementing standard care rather than replacing it.
2. Shockwave Therapy: Basic Principles
2.1 What Is Shockwave Therapy?
Shockwave therapy, clinically known as extracorporeal shockwave therapy (ESWT), utilizes high-energy acoustic waves to deliver mechanical stimulation to targeted tissues. Initially developed for lithotripsy, shockwave technology has since expanded into musculoskeletal medicine and regenerative therapies.
In wound care applications, low- to medium-energy shockwaves are applied to surrounding tissues rather than directly into the wound bed. These acoustic pulses generate mechanical stress that activates mechanotransduction pathways, triggering a cascade of biological responses associated with tissue repair.
2.2 How Shockwaves Interact with Biological Tissue
Shockwaves exert both physical and biochemical effects. The rapid pressure fluctuations induce micro-deformation within cells and the extracellular matrix, stimulating mechanosensitive receptors. This mechanical input is translated into biochemical signals that influence gene expression, protein synthesis, and cellular behavior.
Additionally, cavitation effects produced by shockwaves enhance membrane permeability and promote the release of signaling molecules. These processes collectively contribute to angiogenesis, cell proliferation, and tissue remodeling, forming the mechanistic foundation for shockwave-supported wound healing.
3. Mechanisms of Shockwave Therapy in Wound Healing
3.1 Enhancing Local Blood Flow and Microcirculation
Adequate perfusion is fundamental to wound healing, as oxygen and nutrient delivery directly influence cellular metabolism and immune function. Chronic wounds frequently suffer from microvascular impairment, resulting in tissue hypoxia. Shockwave therapy has been shown to stimulate angiogenic factors such as vascular endothelial growth factor (VEGF) and endothelial nitric oxide synthase (eNOS).
By promoting neovascularization and vasodilation, shockwave therapy improves local microcirculation. This enhanced blood flow facilitates oxygen diffusion, nutrient transport, and metabolic waste removal, creating a microenvironment more conducive to tissue regeneration.
3.2 Stimulating Cellular Regeneration and Tissue Repair
Fibroblasts, keratinocytes, and endothelial cells are central to wound repair. In chronic wounds, these cells often exhibit reduced proliferative capacity. Shockwave-induced mechanical stimulation activates intracellular signaling pathways that promote fibroblast proliferation, collagen synthesis, and extracellular matrix deposition.
Furthermore, shockwave therapy may facilitate the recruitment and differentiation of progenitor cells, supporting granulation tissue formation and epithelial migration. This regenerative stimulation helps reinitiate the proliferative phase of healing that is often stalled in chronic wounds.
3.3 Modulating Chronic Inflammation
Persistent inflammation is a hallmark of chronic wounds, characterized by excessive cytokine release and protease activity. Shockwave therapy appears to modulate inflammatory responses by influencing macrophage polarization and reducing pro-inflammatory mediator expression.
This immunomodulatory effect supports the transition from chronic inflammation toward a regulated healing response, allowing tissue repair mechanisms to proceed more effectively.
4. Wounds That May Benefit from Shockwave Therapy
4.1 Long-Standing Ulcers Resistant to Conventional Care
When chronic ulcers show minimal improvement despite optimized care, this lack of progress often indicates severe underlying microcirculatory deficits and impaired cellular signaling. Shockwave therapy provides a biological stimulus that can complement existing treatments by targeting these underlying deficiencies.
Such ulcers may benefit from enhanced angiogenesis and cellular activation, particularly when standard interventions alone fail to produce sufficient granulation tissue or wound contraction.
4.2 Delayed Healing in Post-Surgical Wounds
Surgical wounds may become chronic when tissue perfusion is compromised or when excessive tension disrupts healing. Shockwave therapy applied to peri-wound tissues can support vascular remodeling and cellular repair processes, helping restore normal healing trajectories.
By improving the biological environment around the incision site, shockwave therapy may reduce healing time and lower the risk of secondary complications.
4.3 Wounds Associated with Circulatory Impairment
Ischemic wounds linked to vascular insufficiency present a significant therapeutic challenge. Shockwave therapy, by stimulating angiogenesis and improving blood flow, directly addresses the core perfusion deficits that limit the effectiveness of conventional treatments in these contexts.
5. Treatment Process and Clinical Considerations
5.1 General Treatment Workflow
Clinicians typically administer shockwave therapy as part of a structured wound care program in outpatient or clinical settings. They adjust key treatment parameters—such as energy level and pulse frequency—based on the specific wound characteristics and the patient’s tolerance, scheduling sessions weekly or biweekly over a course of several weeks.
Crucially, this therapy integrates with standard wound management practices rather than functioning in isolation. This approach ensures comprehensive, synergistic care.
5.2 Safety, Contraindications, and Complementary Therapies
Shockwave therapy is generally well tolerated, with minimal adverse effects when applied correctly. Contraindications include active malignancy in the treatment area, uncontrolled infection, and certain vascular abnormalities. Clinical judgment is essential to ensure patient safety.
Laser therapy, particularly low-level laser therapy (LLLT), is sometimes used alongside shockwave therapy. While laser therapy employs photobiomodulation to influence cellular metabolism, shockwave therapy relies on mechanical stimulation. These modalities may offer complementary biological effects when integrated into a multidisciplinary approach.
FAQ
Is shockwave therapy painful for chronic wound patients?
Most patients experience mild discomfort rather than pain. Sensation typically decreases as treatment progresses.
Can shockwave therapy replace traditional wound care?
No. It should be used as an adjunct to comprehensive wound management.
How long before results are noticeable?
Biological changes may begin early, but visible wound improvement typically occurs over several weeks.
Is shockwave therapy suitable for home use?
Clinical-grade shockwave therapy should be administered by trained professionals using certified devices.
How does shockwave therapy differ from laser therapy?
Shockwave therapy uses mechanical acoustic energy, while laser therapy relies on light-based photobiomodulation. Both aim to stimulate healing via different mechanisms.
Conclusion
Shockwave therapy represents a scientifically grounded, non-invasive adjunct in the management of chronic wounds. By enhancing microcirculation, stimulating cellular regeneration, and modulating inflammation, it addresses key biological barriers that hinder healing. When integrated into evidence-based wound care protocols and complemented by modalities such as laser therapy, shockwave therapy offers meaningful potential to improve outcomes for patients with chronic, non-healing wounds.
Références
Schaden W, Fischer A, Sailler A. Extracorporeal shock wave therapy of nonunion or delayed osseous union. Clinical Orthopaedics and Related Research.
https://pubmed.ncbi.nlm.nih.gov/11603349
Stojadinovic O, et al. Cellular and molecular characteristics of chronic wounds. Acta Dermato-Venereologica.
https://pubmed.ncbi.nlm.nih.gov/18931421
Folkman J. Angiogenesis in wound healing. Journal of Investigative Dermatology.
https://pubmed.ncbi.nlm.nih.gov/7541477
Hamblin MR. Mechanisms and applications of photobiomodulation therapy. AIMS Biophysics.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5607802
Wollina U. Low-level laser therapy in wound healing. Journal of Cosmetic and Laser Therapy.
