Introduction
Muscle inflammation is a common yet often underestimated cause of persistent pain, stiffness, and functional limitation. From athletes and physically demanding professions to individuals with sedentary lifestyles, localized muscle inflammation can significantly impair daily activities and quality of life. When inflammation becomes chronic or recurrent, it may progress into myositis—a condition that is frequently resistant to conventional treatment approaches. As patients and clinicians seek non-invasive, evidence-based alternatives, shockwave therapy has emerged as a modern solution for managing muscle inflammation and myositis. By addressing underlying biological processes such as impaired circulation, tissue adhesion, and inflammatory signaling, this therapy offers a targeted approach that supports long-term recovery rather than temporary symptom suppression.
1. Understanding Muscle Inflammation and Myositis
Before exploring how shockwave therapy works, it is essential to understand the nature of muscle inflammation and myositis. These conditions involve complex physiological processes that go beyond simple muscle soreness.
1.1 What Is Muscle Inflammation?
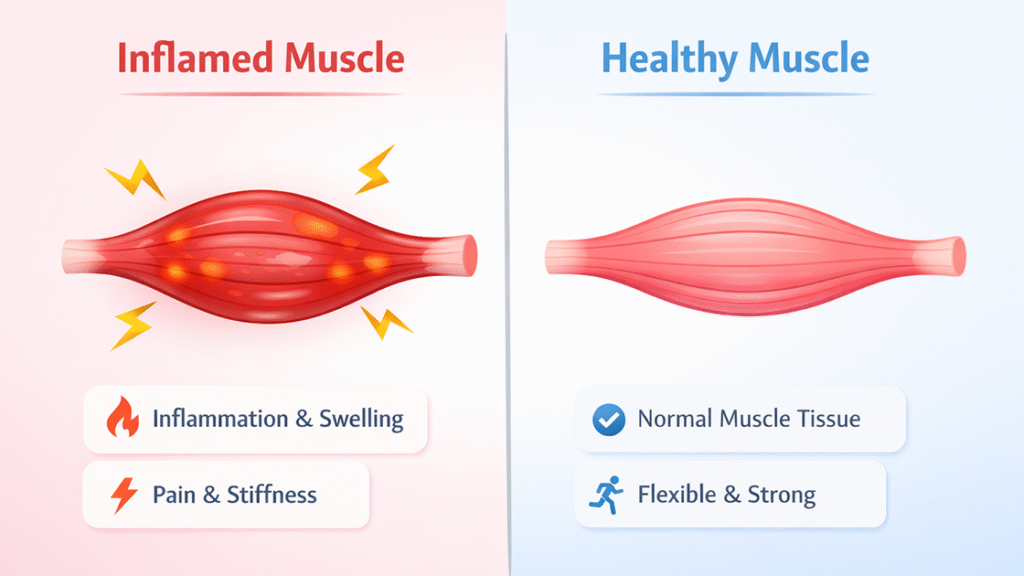
Muscle inflammation refers to a localized inflammatory response within muscle tissue, typically characterized by pain, swelling, tenderness, and reduced mobility. At the cellular level, inflammation involves the release of cytokines and other inflammatory mediators that alter tissue metabolism and pain sensitivity.
While acute inflammation is a natural and protective response to injury, prolonged inflammation can disrupt tissue healing. Chronic muscle inflammation often leads to fibrosis, reduced elasticity, and persistent discomfort, creating a cycle of pain and functional impairment.
1.2 Common Causes of Myositis
Myositis can develop from a variety of causes, most commonly related to mechanical stress and tissue overload. Repetitive movements, overtraining, poor posture, and unresolved muscle injuries are frequent contributors. In some cases, localized trauma or microtears can trigger ongoing inflammatory responses.
Reduced blood supply, metabolic inefficiency, and inadequate tissue regeneration further contribute to the persistence of inflammation. When these factors are not adequately addressed, muscle tissue remains vulnerable to reinjury and chronic pain.
1.3 Symptoms and Functional Limitations
Patients with muscle inflammation or myositis commonly experience deep, localized pain, stiffness, and sensitivity to touch. Symptoms may worsen with activity or prolonged static positions, limiting strength, flexibility, and endurance.
Over time, these limitations can interfere with work performance, athletic training, and daily mobility. The psychological impact of chronic discomfort often adds to the overall burden, emphasizing the need for effective and sustainable treatment strategies.
2. Limitations of Conventional Treatments for Muscle Inflammation
Traditional management strategies for muscle inflammation aim to reduce pain and inflammation, but they often fail to address the underlying biological factors that sustain the condition.
2.1 Rest, NSAIDs, and Physical Therapy
Initial treatment typically includes rest, nonsteroidal anti-inflammatory drugs (NSAIDs), and physical therapy. While these approaches may provide short-term relief, their effectiveness often diminishes in chronic cases.
NSAIDs can reduce inflammation temporarily but do not promote tissue regeneration. Physical therapy remains essential but may be limited when pain restricts active participation or when deep tissue inflammation persists despite rehabilitation efforts.
2.2 Injection-Based Treatments and Their Risks
In some cases, corticosteroid injections are used to suppress inflammation. Although injections may reduce pain rapidly, their effects are often temporary. Repeated injections can weaken soft tissues, impair healing, and increase the risk of further injury.
For patients with chronic myositis, reliance on injection-based treatments may delay meaningful recovery rather than restore normal muscle function.
2.3 Why Chronic Muscle Inflammation Often Persists
One of the primary reasons muscle inflammation becomes chronic is inadequate circulation and tissue metabolism. Inflamed muscle tissue often exhibits poor oxygen delivery, limited nutrient exchange, and accumulation of metabolic waste products.
Without addressing these underlying issues, conventional treatments may control symptoms but fail to create the biological environment necessary for long-term healing.
3. What Is Shockwave Therapy?
Shockwave therapy is a non-invasive treatment modality that has gained widespread use in musculoskeletal medicine. Its application in muscle inflammation and myositis is supported by growing clinical and scientific interest.
3.1 Overview of Shockwave Therapy Technology
Shockwave therapy uses high-energy acoustic waves that are transmitted into targeted tissues. These waves generate controlled mechanical stimulation that interacts with soft tissues at both the cellular and structural levels.
Unlike thermal modalities, this therapy does not rely on heat. Instead, it delivers mechanical energy that triggers biological responses, making it suitable for treating chronic inflammatory conditions.
3.2 How Shockwave Therapy Interacts with Muscle Tissue
When shockwaves reach muscle tissue, they create micro-mechanical stress that stimulates local biological activity. This interaction enhances cellular signaling pathways involved in inflammation regulation, circulation, and tissue remodeling.
By targeting deep muscle layers, shockwave therapy can address pathological changes that are often inaccessible to surface-level treatments.
4. How Shockwave Therapy Treats Muscle Inflammation
The therapeutic effects of shockwave therapy extend beyond symptom relief. Its mechanisms directly support tissue recovery and functional restoration.
4.1 Reducing Local Inflammatory Response
Shockwave therapy helps modulate inflammatory mediators by influencing cytokine expression and cellular signaling. This regulation reduces excessive inflammation while preserving the body’s natural healing response.
As inflammation subsides, pain sensitivity decreases, allowing patients to move more freely and engage more effectively in rehabilitation.
4.2 Improving Blood Circulation and Oxygen Supply
One of the most critical benefits of shockwave therapy is its ability to enhance microcirculation. Improved blood flow increases oxygen delivery and nutrient availability while facilitating the removal of inflammatory byproducts.
This improved circulation creates a healthier tissue environment that supports healing and reduces the likelihood of inflammation recurrence.
4.3 Breaking Down Soft Tissue Adhesions and Trigger Points
Chronic muscle inflammation is often associated with myofascial adhesions and trigger points. Shockwave therapy mechanically disrupts these dysfunctional tissue patterns, restoring normal muscle elasticity and movement.
Releasing adhesions reduces abnormal muscle tension and improves overall tissue mobility.
4.4 Stimulating Tissue Regeneration
Shockwave therapy promotes cellular activity involved in tissue repair, including fibroblast stimulation and collagen remodeling. These regenerative effects support stronger, more resilient muscle tissue over time.
For patients with chronic myositis, this regenerative stimulus is essential for lasting improvement.
5. Clinical Applications for Muscle Inflammation
Shockwave therapy is applied across a wide range of clinical scenarios involving muscle inflammation and myositis.
5.1 Shockwave Therapy for Sports-Related Muscle Inflammation
Athletes frequently experience muscle inflammation due to overuse, repetitive strain, and high training loads. Shockwave therapy supports faster recovery by reducing inflammation and restoring muscle function.
Its non-invasive nature allows athletes to continue training with minimal interruption while addressing underlying tissue stress.
5.2 Shockwave Therapy for Occupational Muscle Overuse
Individuals with physically demanding jobs or prolonged static postures often develop localized muscle inflammation. Shockwave therapy effectively targets these areas, improving mobility and reducing work-related discomfort.
This application is particularly valuable for patients who have not responded adequately to conventional therapies.
5.3 Chronic Myositis and Recurrent Muscle Pain
For patients with long-standing or recurrent myositis, shockwave therapy offers a solution that addresses both symptoms and root causes. By improving circulation and tissue quality, it reduces the frequency and severity of flare-ups.
6. What to Expect During Shockwave Therapy Treatment
Understanding the treatment process helps patients approach shockwave therapy with realistic expectations.
6.1 Treatment Session Process
During a session, a handheld applicator delivers acoustic waves to the affected muscle area. Treatment typically lasts 10 to 15 minutes, depending on the size and location of the tissue involved.
The procedure is performed in an outpatient setting and does not require anesthesia.
6.2 Treatment Frequency and Duration
Most treatment protocols involve one session per week over three to six weeks. The exact schedule depends on the severity and chronicity of the inflammation.
Gradual improvement is commonly observed as tissue responses accumulate over successive sessions.
6.3 Sensations and Patient Experience
Patients may feel mild to moderate discomfort during treatment, particularly in sensitive areas. However, sensations are generally well tolerated and decrease as inflammation resolves.
Post-treatment soreness is typically mild and temporary.
7. Safety, Contraindications, and Patient Selection
Proper patient selection and clinical oversight ensure safe and effective outcomes.
7.1 Is Shockwave Therapy Safe for Muscle Inflammation?
When applied by trained professionals, shockwave therapy has a strong safety profile. It is non-invasive and does not involve pharmaceuticals or injections.
7.2 Who Is an Ideal Candidate?
Patients with chronic or recurrent muscle inflammation who have not responded fully to conventional treatments are often ideal candidates. Active individuals seeking functional recovery rather than temporary relief also benefit significantly.
7.3 When Shockwave Therapy May Not Be Recommended
Shockwave therapy may not be suitable for individuals with bleeding disorders, acute infections at the treatment site, or certain neurological conditions. A thorough clinical assessment is essential prior to treatment.
FAQ
Does shockwave therapy worsen muscle inflammation?
When applied correctly, shockwave therapy helps regulate inflammation rather than exacerbate it.
How soon can improvement be expected?
Many patients notice improvement within a few sessions, with continued progress over the treatment course.
Can shockwave therapy be combined with physical therapy?
Yes. Combining shockwave therapy with rehabilitation exercises often enhances overall outcomes.
Conclusion
Shockwave therapy represents a modern, non-invasive approach to managing muscle inflammation and myositis. By improving circulation, regulating inflammation, and stimulating tissue regeneration, it addresses the underlying causes of chronic muscle pain rather than merely suppressing symptoms.
For patients seeking sustainable recovery and functional improvement, this therapy offers a clinically supported pathway toward long-term relief.
Références
Shockwave Therapy in Musculoskeletal Disorders
https://pubmed.ncbi.nlm.nih.gov/30810279
Biological Effects of Extracorporeal Shockwave Therapy
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6029704
Clinical Indications for Shockwave Therapy
