Introduction
Neurological conditions affecting muscle tone and movement control represent some of the most challenging aspects of modern healthcare. Among these conditions, hypertonia and dystonia significantly impact patients’ quality of life, limiting their independence and daily functioning. Traditional therapeutic approaches, while beneficial, often fall short of providing complete symptom management, leaving patients and healthcare providers searching for innovative solutions.
What Are Hypertonia and Dystonia in Simple Terms?
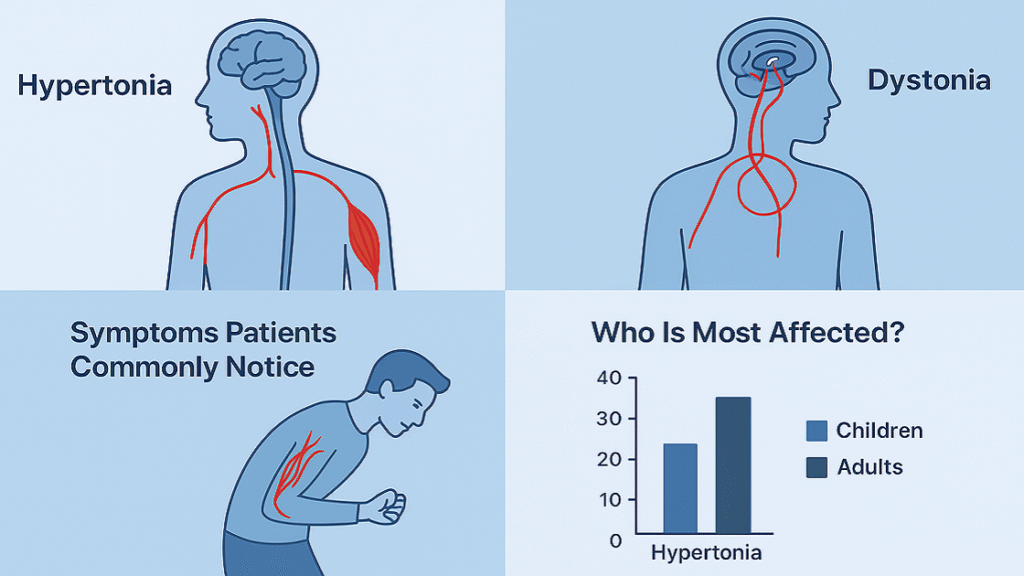
Hypertonia is a neurological condition where muscle tone is abnormally increased, leading to stiffness, rigidity, and resistance to movement. Muscles may contract involuntarily even at rest, making voluntary movements difficult and sometimes painful. This can range from affecting a single area to entire limbs, often interfering with daily activities. Patients commonly describe tightness, cramping, and difficulty relaxing muscles. Dystonia, in contrast, is marked by involuntary muscle contractions that cause twisting movements and abnormal postures. It may affect one region (like the neck or hands) or multiple muscle groups throughout the body. Unlike hypertonia’s constant stiffness, dystonia symptoms are often triggered by certain activities or positions, making them unpredictable and disabling. The underlying problem lies in the basal ganglia and related neural networks that control movement. While both conditions involve abnormal muscle activity, their patterns and triggers differ, which impacts treatment strategies.
Why Current Treatments Don’t Always Work
Standard treatments for hypertonia and dystonia include medications, botulinum toxin injections, baclofen pumps, and surgery. While these options can help, they often come with limitations. Oral medications may reduce symptoms but frequently cause side effects such as drowsiness, weakness, and cognitive changes. Over time, patients may also develop tolerance, reducing effectiveness. Botulinum toxin injections are useful for localized symptoms, but results vary and treatments must be repeated every few months. Some patients also stop responding over time due to antibody formation. Baclofen pumps or surgical options like deep brain stimulation may work for severe cases, but these approaches are invasive, carry risks, and require long recovery. Because of these challenges, many patients find traditional therapies either too burdensome or only partially effective. This treatment gap has fueled interest in safer, non-invasive alternatives that can offer lasting relief with fewer side effects.
Shockwave Therapy: A New Option Patients Are Asking About
Extracorporeal shockwave therapy (ESWT) is an emerging non-invasive treatment showing promise for hypertonia and dystonia. First used for kidney stones, it is now applied in orthopedics, wound care, and neurological conditions. Since the late 1990s, focused shockwave therapy has been reported to reduce abnormal muscle tone. The therapy uses high-energy sound waves to stimulate healing, reduce inflammation, and influence neural pathways that regulate movement. Unlike medications, which act on the whole body, shockwave therapy targets specific muscles. This localized effect reduces the risk of systemic side effects while preserving normal muscle function elsewhere. Sessions are quick, minimally painful, and carry a favorable safety profile compared to injections or surgery. Patients appreciate that it may offer longer-lasting relief without repeated invasive procedures. As a result, ESWT is increasingly viewed as a valuable alternative or complement to standard treatments for managing muscle stiffness and abnormal movements.
Who This Guide Is for (Patients, Families, and Professionals)
This comprehensive guide serves multiple stakeholders in the healthcare ecosystem, each with unique information needs and perspectives. For patients living with hypertonia or dystonia, this resource provides evidence-based information about shockwave therapy’s potential benefits, risks, and realistic expectations. Understanding treatment options empowers patients to engage in informed discussions with their healthcare providers and make decisions aligned with their personal goals and preferences. Family members and caregivers will find valuable insights into the practical aspects of shockwave therapy, including treatment logistics, potential outcomes, and how this intervention might fit into comprehensive care plans. Healthcare professionals, including physiatrists, neurologists, physical therapists, and occupational therapists, can utilize this guide to stay current with emerging treatment modalities and evidence-based applications of shockwave therapy in neurological rehabilitation.
Understanding Hypertonia and Dystonia
The complexity of movement disorders requires a thorough understanding of their underlying pathophysiology, clinical presentations, and impact on patients’ lives. Both hypertonia and dystonia represent disruptions in the normal neural control of movement, albeit through different mechanisms and with distinct clinical manifestations.
What Causes Hypertonia?
Hypertonia occurs when the central nervous system’s motor pathways, especially upper motor neurons, are damaged. This disrupts the balance of excitatory and inhibitory signals, causing persistent muscle stiffness. Common causes include cerebral palsy, where early brain injury leads to lifelong spasticity; stroke, where corticospinal tract damage results in abnormal tone; and spinal cord injury, which removes inhibitory control from higher brain centers. Multiple sclerosis also frequently causes hypertonia, as demyelination and inflammation interfere with nerve signaling, leading to pain, spasticity, and loss of mobility. Traumatic brain injuries may produce similar effects depending on the location and severity of damage. In all cases, the result is involuntary, exaggerated muscle tone that reduces movement efficiency and complicates daily activities. Newer treatments such as radial shockwave therapy (RSWT) have shown promise in easing stiffness and improving function without significant side effects, particularly in patients with multiple sclerosis.
What Causes Dystonia?
Dystonia is caused by dysfunction within the basal ganglia-thalamo-cortical circuits, which regulate movement. In primary dystonia, genetic mutations such as DYT1 or DYT6 alter neurotransmission and motor control. Secondary dystonia can follow stroke, traumatic brain injury, infections, metabolic disorders, or reactions to certain drugs. It also appears in Parkinson’s disease, often affecting the hands or feet. The condition is linked to abnormal dopamine signaling, impaired sensory feedback, and loss of inhibition in motor pathways. Recent research highlights the cerebellum’s role, suggesting dystonia involves broader network dysfunction rather than just basal ganglia damage. Symptoms may be triggered or worsened by fatigue, stress, or specific activities, which explains why some patients experience task-related dystonias, such as writer’s cramp or musician’s dystonia. The complexity of these neural disruptions makes dystonia highly variable, with both genetic and environmental factors influencing its onset, severity, and responsiveness to treatment.
Symptoms Patients Commonly Notice
Hypertonia causes muscle stiffness, pain, and reduced range of motion.
Walking, stretching, and fine motor tasks become increasingly difficult.
Children with cerebral palsy may show toe-walking or scissoring gait.
Stroke and MS patients often struggle with coordination and mobility.
Symptoms may worsen at night, disrupting sleep.
Dystonia leads to involuntary twisting movements and abnormal postures.
Cervical dystonia causes head tilting or turning.
Blepharospasm forces eyelids to close involuntarily.
Oromandibular dystonia affects speech and swallowing.
Focal hand dystonia interferes with writing or playing music.
Unpredictable movements often cause anxiety and social withdrawal.
Who Is Most Affected?
Hypertonia can occur at any age, but its causes vary. In children, cerebral palsy is the main cause, affecting about 2–3 per 1,000 live births. In adults, post-stroke spasticity appears in up to 40% of survivors within months, while multiple sclerosis leads to hypertonia in nearly 80% of patients during disease progression. Spinal cord and traumatic brain injuries are also common sources, often producing lasting stiffness below the injury site. Dystonia affects around 16.4 per 100,000 people, ranking as the third most common movement disorder after Parkinson’s disease and essential tremor. Cervical dystonia is the most frequent focal type, usually appearing in middle-aged women. Generalized dystonia often starts in childhood or adolescence, while secondary forms can appear at any age depending on the cause. Occupational dystonias affect people with repetitive fine motor tasks—such as musicians, writers, and craftsmen—showing how both biological and environmental factors contribute.
La thérapie par ondes de choc expliquée
Understanding the mechanism and applications of shockwave therapy provides crucial context for evaluating its potential in treating movement disorders. This non-invasive technology harnesses the power of acoustic waves to stimulate healing and potentially modify neural function.
What Exactly Is Shockwave Therapy?
Shockwave therapy, or extracorporeal shockwave therapy (ESWT), is a non-invasive treatment that uses high-energy acoustic waves on targeted body areas. First developed to break up kidney stones, it is now widely used in musculoskeletal medicine, rehabilitation, and neurology. The shockwaves trigger biological responses that improve blood flow, reduce inflammation, and stimulate tissue repair. Treatments may involve focused shockwaves for deep penetration or radial shockwaves for broader, surface-level effects. Unlike medications or surgery, shockwave therapy works locally, reducing the risk of systemic side effects. Sessions are short, outpatient-based, and typically require no anesthesia, though mild discomfort may occur. Recovery is immediate, making it practical and well tolerated. More recently, research has explored its role in neurological conditions such as hypertonia and dystonia, where it may help regulate abnormal muscle tone. With growing clinical evidence and a favorable safety profile, shockwave therapy is emerging as a promising, patient-friendly option.
How It Works on Muscles and Nerves
Shockwave therapy works by transmitting mechanical sound waves into tissues, where they trigger biological and neurological responses. On a muscular level, the shockwaves improve blood circulation, reduce local inflammation, and stimulate tissue repair by activating cellular pathways that promote healing. They can also reduce muscle tightness by breaking down fibrotic tissue and improving flexibility. On a neurological level, shockwaves are believed to modulate nerve signaling within the central and peripheral nervous systems. This may help restore balance between excitatory and inhibitory signals, reducing abnormal muscle contractions. For patients with hypertonia or dystonia, this means fewer involuntary spasms, improved range of motion, and greater comfort in daily activities. Unlike systemic medications, which affect the entire body, shockwave therapy acts directly at the problem site. This targeted approach allows for precise treatment with minimal side effects, making it especially attractive for long-term management of chronic neuromuscular conditions.
Conditions Where Shockwave Therapy Is Already Used
Shockwave therapy has been widely adopted in orthopedics, sports medicine, and rehabilitation for over two decades. It is best known for treating chronic tendon and ligament injuries such as plantar fasciitis, tennis elbow, Achilles tendinopathy, and rotator cuff injuries. In orthopedics, it helps stimulate bone healing in cases of delayed fracture union. In wound care, shockwave therapy improves blood flow and tissue repair, accelerating healing in chronic ulcers and diabetic foot wounds. More recently, it has gained attention in neurological rehabilitation, where studies show benefits in reducing spasticity in stroke, cerebral palsy, multiple sclerosis, and spinal cord injuries. Patients often report reduced stiffness, improved mobility, and better quality of life after treatment. Because of its versatility and non-invasive nature, shockwave therapy is considered an attractive alternative when standard treatments such as medication, injections, or surgery are ineffective or poorly tolerated.
Is It Safe? Who Should Avoid It?
Shockwave therapy is generally considered safe, non-invasive, and well-tolerated when performed by trained professionals. Most patients experience only mild side effects such as temporary soreness, redness, or slight swelling in the treated area, which usually resolve within a few days. Unlike medications, shockwave therapy does not cause systemic side effects such as drowsiness or organ toxicity. However, not everyone is a suitable candidate. It should be avoided in individuals with blood clotting disorders, active infections, tumors, or open wounds in the treatment area. Patients with pacemakers or other implanted electronic devices may also need clearance before undergoing therapy. Pregnant women are generally advised to avoid the treatment as a precaution. Overall, when proper screening and guidelines are followed, shockwave therapy is considered a safe and effective treatment option for many musculoskeletal and neurological conditions, offering patients a low-risk alternative to more invasive procedures.
Shockwave Therapy for Hypertonia
The application of shockwave therapy specifically for hypertonia management represents an evolving field with promising preliminary results and growing clinical interest among rehabilitation professionals.
Ce que dit la recherche
Current research supports shockwave therapy for hypertonia across cerebral palsy, stroke, multiple sclerosis, and other neurological conditions. In children with cerebral palsy, studies show significant gains in muscle tone, range of motion, and functional mobility. Adult trials also report reduced hypertonia following treatment. In stroke patients, shockwave therapy improves spasticity scores and functional outcomes, with effects lasting for months. Evidence in multiple sclerosis is especially strong, with randomized controlled trials demonstrating measurable reductions in muscle tone and sustained benefits for up to 24 weeks. Beyond reducing stiffness, studies consistently highlight improvements in pain relief, mobility, and quality of life. These results position shockwave therapy as a promising non-invasive option for patients struggling with spasticity. However, most trials involve small sample sizes, underscoring the need for larger, high-quality studies to confirm long-term effectiveness and establish standardized treatment protocols.
How Patients Benefit: Flexibility, Mobility, and Pain Relief
Patients receiving shockwave therapy for hypertonia often notice benefits that go beyond reduced muscle tone. One of the most consistent outcomes is an increased range of motion, making daily tasks such as transfers, dressing, and grooming easier. Improved flexibility also helps prevent contractures and enhances independence in self-care. Many patients report better mobility, including more efficient and natural walking patterns with less energy expenditure. Another important benefit is pain relief, particularly for those with chronic discomfort caused by constant muscle contractions and joint stress. Together, reduced stiffness, greater flexibility, and decreased pain create a synergistic effect that improves overall functional ability. These changes not only make movements smoother but also reduce fatigue, allowing patients to engage more fully in daily life. Many individuals describe feeling more confident and capable, highlighting shockwave therapy’s potential to enhance both physical function and quality of life.
How Long the Results Last
The duration of therapeutic benefits following shockwave therapy varies among individuals and depends on multiple factors including underlying condition severity, treatment parameters, and concurrent interventions. Most clinical studies report sustained improvements lasting 12-24 weeks following completed treatment courses, with some patients experiencing benefits for up to six months. The durability of effects appears related to the mechanism of action, as structural changes in muscle and connective tissue may provide longer-lasting benefits compared to purely neurological interventions. Individual factors influencing treatment durability include age, overall health status, disease severity, and adherence to recommended follow-up care including physical therapy and exercise programs. Patients who maintain active lifestyle modifications and continue appropriate rehabilitation interventions tend to experience more prolonged benefits. Some individuals may benefit from periodic maintenance treatments, though optimal retreatment intervals remain under investigation. The ability to repeat treatments safely provides flexibility in long-term management strategies for chronic conditions.
Shockwave Therapy for Dystonia
The application of shockwave therapy in dystonia management represents a relatively newer therapeutic frontier, with emerging evidence suggesting potential benefits for this complex movement disorder.
Current Clinical Evidence
Research on shockwave therapy for dystonia is still developing, but early findings are positive. ESWT appears effective and safe for upper limb dystonia, especially secondary types. Most studies focus on focal dystonias such as cervical dystonia and upper limb involvement, showing improved movement quality and functional performance. Standard dystonia rating scales are commonly used to measure progress. In Parkinson’s disease-related dystonia, immediate improvements in tone and movement have been observed after treatment. Studies by Ni et al. (2024) and Huang et al. (2022) showed that combining botulinum toxin with shockwave therapy for foot dystonia in PD normalized plantar pressure and improved balance and lower limb function. Despite these encouraging results, evidence remains limited, as most trials involve small sample sizes and short follow-up. Larger, long-term randomized controlled trials are needed to confirm effectiveness and define optimal treatment protocols.
Improvements in Muscle Control and Daily Function
Shockwave therapy can help dystonia patients regain better voluntary muscle control and coordination. By reducing involuntary contractions, it allows smoother, more purposeful movements. For example, patients with focal hand dystonia may improve their writing, while those with cervical dystonia may gain better head alignment and reduced twisting. Such changes improve work tasks, hobbies, and daily living skills. The therapy is especially useful in task-specific dystonias—like writer’s cramp or musician’s dystonia—helping restore some professional ability, even if full recovery is rare. With improved control, patients reduce compensatory movements that previously caused inefficiency and fatigue. This leads to more natural movement and less physical strain. Beyond physical benefits, regaining function improves confidence, lowers anxiety about unpredictable symptoms, and enhances overall wellbeing. These psychological gains are often as valuable as the physical improvements.
Real-Life Quality of Life Changes for Patients
The benefits of shockwave therapy extend into daily life and emotional health. Reduced visible dystonic movements help patients feel less self-conscious, encouraging greater participation in social and community activities. Many report better job opportunities or a return to tasks they had abandoned due to dystonia, particularly in occupational forms. Improved sleep is another common benefit, as reduced nighttime movements enhance rest, energy, and mood. At home, patients may require less assistance with activities, reducing stress and improving family relationships. These functional gains also strengthen independence and reduce frustration. Psychologically, patients often experience higher self-esteem, less depression, and greater confidence in managing their condition. Such improvements motivate continued rehabilitation and support a more active lifestyle. Overall, shockwave therapy can provide meaningful quality of life changes that extend well beyond clinical measures.
Practical Considerations for Patients and Caregivers
Understanding the practical aspects of shockwave therapy helps patients and families make informed decisions and prepare appropriately for treatment experiences.
Who Might Be a Good Candidate?
Ideal candidates for shockwave therapy include people with focal or regional hypertonia or dystonia who have not achieved sufficient relief from conventional treatments. Those experiencing medication side effects or seeking alternatives to invasive procedures are also suitable. Functional impairment affecting daily activities, work, or quality of life strengthens the case for treatment, particularly when symptoms are localized and treatable. Candidates must be medically stable, with adequate cardiovascular health and absence of conditions that could complicate therapy. Realistic expectations are crucial, as the therapy improves symptoms rather than providing a cure. Motivation to participate in concurrent rehabilitation enhances outcomes. Pediatric patients must be cooperative, while elderly patients may respond differently. Overall, suitability depends on symptom type, severity, patient health, and willingness to engage in complementary rehabilitation strategies.

What a Typical Treatment Session Looks Like
A shockwave therapy session begins with patient assessment and positioning to ensure comfort and precise treatment. Targeted areas are identified via palpation or ultrasound guidance, and the skin is cleaned with coupling gel applied. Most patients remain clothed except for the treatment area. The shockwave applicator delivers pulses at specified energy levels, usually lasting 15–30 minutes depending on treated regions and protocols. Patients often feel tolerable discomfort similar to deep tissue massage. Continuous communication allows adjustments to optimize comfort. After the session, providers assess immediate side effects and give aftercare instructions. Sessions are outpatient, non-invasive, and do not require anesthesia, enabling quick recovery. Repeated sessions may be recommended based on condition severity and response.
Possible Side Effects and How to Manage Them
Shockwave therapy side effects are usually mild and short-lived, resolving within 24–48 hours. Common effects include skin redness, mild swelling, localized tenderness, or bruising, which can be managed with ice packs or over-the-counter anti-inflammatories. Some patients may experience temporary worsening of symptoms during the first 1–2 days, often indicating tissue activation. Rare side effects include transient numbness or altered sensation, typically resolving within days to weeks. Clear patient counseling on expected side effects, symptom monitoring, and proper self-care ensures safety. Most reactions are temporary, non-serious, and manageable, allowing patients to continue therapy with minimal disruption.
Combining Shockwave Therapy with Physical Therapy and Medication
Integrating shockwave therapy with physical therapy enhances outcomes by improving muscle flexibility and reducing tone, allowing more effective stretching, strengthening, and functional training. Reduced resistance helps therapists achieve rehabilitation goals efficiently. Medication adjustments may follow, with potential dose reductions under medical supervision as symptoms improve. Timing coordination with botulinum toxin injections optimizes benefits without interference. Occupational therapy complements these gains through adaptive techniques and environmental modifications, maximizing daily function. Combining these approaches creates synergistic effects, improving mobility, independence, and overall quality of life while addressing both physical and functional limitations.
Real Stories and Expert Opinions
Understanding the practical impact of shockwave therapy through professional perspectives and patient experiences provides valuable insights into the real-world applications and outcomes of this treatment approach.
What Doctors and Therapists Are Saying
Healthcare professionals who have incorporated shockwave therapy into their practice report generally positive experiences and patient outcomes. Physiatrists note that the therapy provides an additional tool in the comprehensive management of movement disorders, particularly for patients who have reached therapeutic plateaus with conventional approaches. The non-invasive nature appeals to both patients and providers, as it avoids the risks and complications associated with surgical interventions while providing meaningful symptom relief. Physical therapists appreciate the enhanced treatment response they observe when combining shockwave therapy with traditional rehabilitation techniques. The reduced muscle tone and improved flexibility following shockwave treatments allow for more effective manual therapy techniques and exercise interventions. Neurologists view the therapy as a promising adjunct to medical management, particularly for patients experiencing medication limitations or side effects. The growing body of research evidence continues to build confidence among healthcare providers regarding the therapy’s safety and efficacy profile.
Patient Stories: Before and After Treatment
Patient testimonials consistently emphasize improvements in functional capacity and quality of life following shockwave therapy interventions. A 45-year-old stroke survivor with severe upper extremity spasticity reported regaining ability to dress independently and perform basic self-care tasks after completing a shockwave treatment course. Her improved arm function allowed return to part-time employment and renewed participation in family activities she had been unable to enjoy since her stroke. A teenager with cerebral palsy experienced significant improvement in walking ability after shockwave therapy targeted to calf muscles. The reduced muscle tone allowed for more normal foot positioning and improved balance, enabling participation in school sports and social activities with peers. Parents reported decreased daily care requirements and improved sleep quality for their child. These stories, while anecdotal, illustrate the potential for meaningful life changes that extend far beyond clinical measurements and objective assessments.
Inspiring Case Examples from Clinics
Clinical centers specializing in movement disorders have documented remarkable cases that demonstrate the therapy’s potential impact. One rehabilitation clinic reported a case series of multiple sclerosis patients who achieved sustained improvements in walking speed and endurance following lower extremity shockwave therapy. These patients were able to reduce assistive device dependence and increase community participation, with benefits lasting over six months post-treatment. A specialized dystonia clinic documented successful treatment of a professional musician with focal hand dystonia who had been unable to perform for over two years. Following a series of targeted shockwave treatments, the patient gradually regained finger dexterity and coordination, eventually returning to professional performance activities. While complete recovery was not achieved, the functional improvement was sufficient to resume career activities with appropriate modifications. Such cases highlight the therapy’s potential to restore meaningful function in highly specific situations.
Conclusion
Shockwave therapy is an emerging, non-invasive treatment offering promise for patients with hypertonia and dystonia, especially those who have not achieved optimal results with conventional therapies. Research supports its safety and efficacy, though larger randomized controlled trials are needed to define optimal protocols and patient selection. Its ability to target specific anatomical regions allows precise treatment while minimizing systemic side effects, and integration with physical or occupational therapy enhances functional improvements. Patients may experience reduced muscle tone, improved mobility, and better quality of life. As clinical experience grows, shockwave therapy could become a standard component of multidisciplinary care for movement disorders. Ongoing research aims to refine treatment parameters, identify ideal candidates, and explore synergistic approaches with medications or rehabilitation. For patients struggling with hypertonia or dystonia, shockwave therapy provides a hopeful, effective option for symptom relief, functional gains, and improved daily living.
References and Trusted Resources
- The Power of Shockwave Therapy for Pain Management
- Shock Waves in the Treatment of Muscle Hypertonia and Dystonia
- Long-Term Effect of Shock Wave Therapy on Upper Limb Hypertonia in Patients Affected by Stroke
- Extracorporeal Shockwave Treatment as Additional Therapy in Patients with Post-Stroke Spasticity of Upper Limb—A Narrative Review
