The gluteal muscles, comprising the powerhouse trio of gluteus maximus, medius, and minimus, serve as the foundation for human locomotion and pelvic stability. When these crucial muscles and their associated tendons become compromised through gluteal tendinopathy, patients often experience debilitating lateral hip pain that can significantly impact their quality of life. This comprehensive guide explores how extracorporeal shockwave therapy (ESWT) has emerged as a revolutionary treatment modality for addressing this challenging condition.
Introduction
Gluteal tendinopathy represents one of the most prevalent causes of lateral hip pain, affecting millions of individuals worldwide, particularly women over 40 years of age. This degenerative condition primarily affects the gluteus medius and minimus tendons where they insert into the greater trochanter of the femur. Understanding the underlying pathophysiology and treatment options is crucial for both healthcare providers and patients seeking effective relief from this often-persistent condition.
What Causes Gluteal Tendinopathy?
Gluteal tendinopathy arises from repeated microtrauma to the gluteal tendons, especially during movements requiring hip abduction and external rotation. This overuse leads to mechanical overload, often triggered by weak hip abductors, poor movement patterns, or prolonged standing. Anatomical risk factors include wide pelvic structure, leg length differences, and altered femoral neck angles. With age, tendons undergo degenerative changes—reduced collagen production and altered extracellular matrix—which lower their resilience. Conditions such as diabetes and thyroid dysfunction can further impair tendon healing. Direct trauma or long periods of immobility can also increase vulnerability. At the cellular level, the condition involves a failed healing response—normal tendon fibers become disorganized, with neovascularization and nerve ingrowth. These changes result in chronic pain and loss of function.
What Are the Different Stages of Gluteal Tendinopathy?
Gluteal tendinopathy develops in progressive stages that influence treatment choice. In the reactive stage, the tendon responds to overload with increased cellular activity. Tendon structure remains intact, and pain occurs during or after activity. The tendon disrepair stage features more disorganized matrix changes. Pain becomes more persistent and may be present even during routine daily movements. Tendons stiffen, and their load tolerance drops. The degenerative stage involves major structural breakdown, cell death, and poor vascular supply. Pain is constant, often interrupting sleep and daily life. Tendons at this stage have limited healing potential and respond poorly to conservative treatments. Recognizing these stages helps tailor interventions to disease severity.
Why This Article Matters
Gluteal tendinopathy is frequently mismanaged with limited success using standard care. Shockwave therapy presents a compelling, evidence-supported alternative. This article aims to explain its scientific basis and clinical relevance. By linking current research with real-world treatment strategies, we help clinicians select ideal candidates and integrate shockwave therapy effectively into rehabilitation plans. This empowers providers to make informed, targeted decisions. Patients also benefit from understanding the therapy’s role, enabling more meaningful discussions with their care team. When well-applied, shockwave therapy improves outcomes, reduces frustration, and helps restore pain-free movement—especially for those with stubborn or advanced tendinopathy.
Shockwave Therapy: Scientific Foundation and Mechanism
The application of mechanical energy for therapeutic purposes has evolved significantly over the past several decades, with extracorporeal shockwave therapy emerging as a sophisticated, non-invasive treatment modality. Understanding the scientific principles underlying this technology is fundamental to appreciating its therapeutic potential in treating gluteal tendinopathy.
What is Extracorporeal Shockwave Therapy (ESWT)?
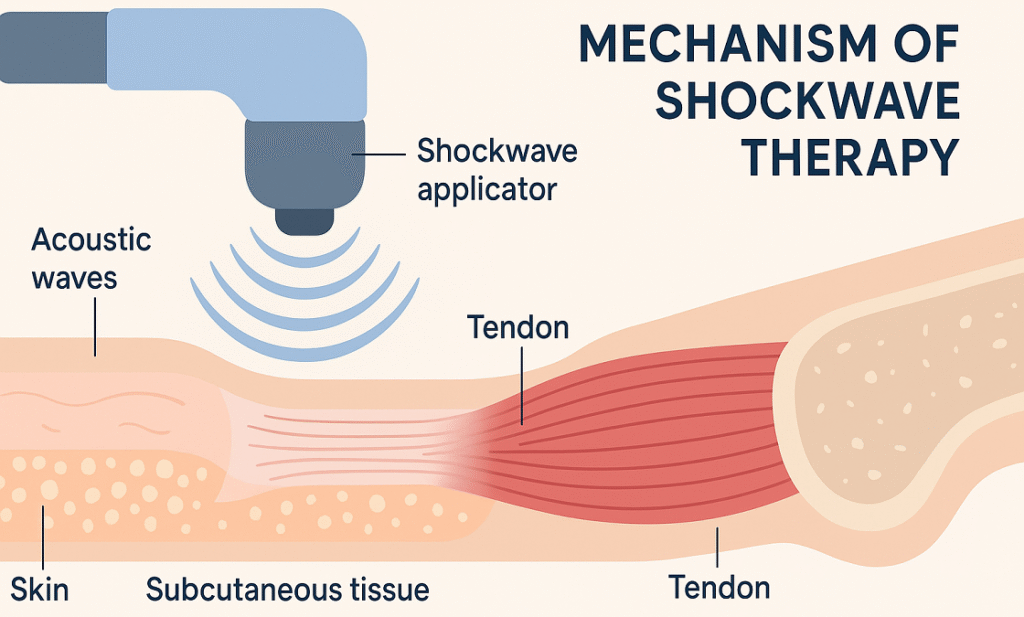
Extracorporeal shockwave therapy (ESWT) is a non-invasive treatment that delivers high-energy acoustic waves to injured tissues. These waves generate rapid pressure shifts, triggering biological responses at the cellular and molecular levels. Two main technologies generate shockwaves: electromagnetic and piezoelectric. Electromagnetic systems use a magnetic field to accelerate a membrane, while piezoelectric systems rely on crystals that deform under electric current, producing precise acoustic waves. During treatment, a handheld applicator is placed over the painful area, with gel ensuring optimal energy transfer. Key parameters—such as energy intensity, pulse rate, and total shocks—are customized based on the injury and patient profile. Most treatment plans require multiple sessions over several weeks. Modern ESWT offers two types: focused shockwaves for deeper, targeted effects and radial shockwaves for broader, surface-level treatment. The choice depends on the injury’s depth and clinical goals.
Biological Mechanisms of Action
The therapeutic efficacy of shockwave therapy stems from its ability to trigger multiple biological processes simultaneously, creating a comprehensive healing response that addresses both the symptoms and underlying pathophysiology of gluteal tendinopathy.
Mechanotransduction and Cellular Response
Mechanotransduction is how cells convert mechanical forces into biochemical signals. When shockwaves hit tendon tissue, they activate mechanosensitive ion channels, triggering cellular pathways that produce key growth factors like VEGF, bFGF, and TGF-β. These promote angiogenesis, cell proliferation, and extracellular matrix formation. Shockwaves also activate nitric oxide pathways, enhancing blood flow and nutrient delivery. Stem and progenitor cells are recruited and differentiate into tenocytes, supporting tendon regeneration. The mechanical forces help align collagen fibers, restoring strength and improving the tendon’s load-bearing capacity.
Neovascularization and Tissue Regeneration
Shockwave therapy boosts neovascularization—new blood vessel formation—in poorly vascularized tendon areas. This is crucial in gluteal tendinopathy, where degeneration often occurs in hypoxic zones. Shockwaves stimulate endothelial cells to form capillaries, enhancing oxygen and nutrient supply while clearing waste and inflammation. They also activate local stem cells and regulate matrix metalloproteinases (MMPs), balancing tissue breakdown and synthesis. This dual action supports the replacement of damaged tendon matrix with healthy tissue, speeding recovery and improving tissue resilience.
Pain Modulation through Gate Control Theory
Shockwave therapy reduces pain partly through gate control theory. The treatment stimulates large-diameter sensory nerve fibers that suppress pain signals from smaller nociceptive fibers, offering immediate relief. It also lowers substance P, a neuropeptide linked to pain, and encourages the release of endogenous opioids. These combined effects help reduce both acute and chronic pain. By addressing peripheral and central pathways, shockwave therapy offers comprehensive pain relief, especially effective for long-standing gluteal tendinopathy.
Collagen Synthesis and Tendon Remodeling
Shockwaves promote tendon healing by stimulating fibroblasts and increasing type I collagen synthesis—the main component of healthy tendons. They also help align new collagen fibers for better tensile strength. The therapy regulates MMPs and their inhibitors, ensuring a balanced process of collagen breakdown and rebuilding. Over time, this controlled remodeling replaces disorganized, damaged tissue with stronger, more elastic tendon fibers, restoring function and resilience.
Scientific Evidence and Research Studies
Shockwave therapy’s efficacy for gluteal tendinopathy is well-supported by clinical research. Meta-analyses and systematic reviews report significant pain relief and improved function compared to placebo. One key randomized controlled trial in The American Journal of Sports Medicine showed a 70% reduction in pain and better function after shockwave treatment, with benefits lasting 12 months and minimal adverse effects. Comparative trials highlight better long-term outcomes than corticosteroid injections, especially in preserving tendon health. Imaging studies, such as ultrasound and MRI, confirm structural tendon healing—showing decreased tendon thickness and normalized echogenicity that align with clinical improvements.
Success Rates and Clinical Outcomes
Shockwave therapy shows success rates between 65% and 85% for gluteal tendinopathy, defined by reduced pain, improved function, and patient satisfaction. Better outcomes are linked to early intervention, younger age, and absence of comorbidities like osteoarthritis. Chronic cases may need more sessions or adjunct therapies. Long-term studies report sustained improvement up to one year post-treatment, though some patients benefit from maintenance sessions, especially those with persistent biomechanical issues.
Where Shockwave Fits in the Treatment Algorithm
The integration of shockwave therapy into the comprehensive management of gluteal tendinopathy requires careful consideration of treatment timing, patient characteristics, and concurrent interventions. Understanding where this modality fits within the broader therapeutic algorithm ensures optimal outcomes while avoiding unnecessary treatments or delays in recovery.
First-Line Treatments: When to Start Conservatively
Conservative management forms the foundation of gluteal tendinopathy treatment, with most clinical guidelines recommending a trial of non-invasive interventions before considering more aggressive options. This approach is based on the principle that many cases of tendinopathy can resolve with appropriate modification of aggravating factors and targeted rehabilitation.
Rest and Activity Modification
Managing gluteal tendinopathy begins with adjusting activities that strain the tendon. Total rest is discouraged, as it may cause muscle weakness and worsen the condition. Instead, the focus is on “relative rest,” which reduces stress on the tendon while maintaining overall movement and fitness. Patients are guided to avoid symptom-provoking actions like prolonged sitting on hard surfaces or repetitive hip abduction. Strategies include modifying daily movements, like stair climbing or car entry, to reduce irritation. Exercise intensity may be lowered by 50–70%, with alternatives chosen to maintain conditioning. As symptoms improve, load is gradually reintroduced using symptom-guided progression to encourage tendon adaptation without aggravation.
NSAIDs and Pain Management
NSAIDs help manage pain in gluteal tendinopathy, though their role in reducing inflammation is limited. Pain relief enables patients to engage in rehab. Topical NSAIDs like diclofenac are often preferred due to fewer systemic side effects. Short-term use (2–4 weeks) during flare-ups is typically effective, but long-term use may hinder tendon healing by affecting prostaglandin and collagen production. Patients with NSAID restrictions can consider acetaminophen, topical capsaicin, or ice therapy. Pain management should be personalized, considering patient history and preferences, with the goal of supporting movement and rehabilitation rather than masking symptoms long-term.
Physical Therapy and Exercise-Based Rehabilitation
Exercise-based rehab is central to treating gluteal tendinopathy. Eccentric strengthening exercises, particularly for hip abduction and external rotation, promote tendon healing by improving collagen structure and load tolerance. The program also targets biomechanical contributors, strengthening the entire lower kinetic chain, including the feet, hips, and core. Rehab begins with isometrics to build early strength, followed by isotonic and functional training. Progressive loading is essential for tissue adaptation. Programs typically last 12–16 weeks, with regular reassessment to tailor progression and ensure effective, goal-driven recovery.
When to Consider Shockwave Therapy?
The decision to incorporate shockwave therapy into the treatment plan requires careful assessment of multiple factors, including symptom duration, response to conservative treatment, and patient-specific characteristics that may influence treatment success.
Duration of Symptoms as a Guide
Shockwave therapy is typically considered after 3–6 months of conservative treatment if symptoms persist. This period allows natural healing while preventing prolonged discomfort. Acute tendinopathy (<3 months) often responds well to rehab alone, but chronic cases may require shockwave’s added biological effects. Individualized timelines are important. If pain remains after 6–8 weeks of proper rehab—or significantly limits daily or work-related function—earlier intervention may be appropriate, especially for athletes or physically demanding jobs. Clinical signs such as prolonged morning stiffness, night pain, or difficulty with basic activities may indicate a need to escalate treatment. Patient goals, symptom burden, and overall quality of life should guide decision-making.
Patient Selection Criteria
Careful patient selection improves shockwave therapy outcomes. Ideal candidates have confirmed gluteal tendinopathy with localized lateral hip pain and supportive imaging. Ages 30–70 respond best, as younger patients may recover conservatively, and older individuals may have more complex degeneration. Contraindications include pregnancy, pacemakers, active cancer, or bleeding disorders. Patients must also have realistic expectations and agree to modify activities during treatment. Psychological factors like fear-avoidance, depression, or catastrophizing can reduce treatment success. Addressing these issues alongside physical care—possibly with mental health support—enhances overall outcomes and patient satisfaction.
Combining Shockwave with Rehabilitation
The synergistic combination of shockwave therapy with structured rehabilitation programs has been shown to produce superior outcomes compared to either intervention alone. This integrated approach leverages the biological effects of shockwave therapy while addressing the biomechanical and functional aspects of recovery through targeted exercise prescription.

Sequential vs. Simultaneous Integration
Rehabilitation can be timed either sequentially or simultaneously with shockwave therapy. Sequential protocols begin with shockwave sessions to reduce pain, followed by rehab once symptoms ease—ideal for patients with high pain levels that hinder exercise. Simultaneous integration delivers shockwave therapy and exercise together. This approach uses mechanical loading from rehab to enhance the biological repair effects of shockwaves. It encourages tissue remodeling and functional improvement through combined stimulation. Recent studies support simultaneous methods, showing better outcomes due to synergy between exercise and shockwave effects. Ultimately, treatment choice depends on symptom severity, patient tolerance, and therapy goals.
Avoiding Common Rehab Mistakes
Rehab errors can undermine shockwave therapy. A common mistake is advancing exercises too quickly after treatment, risking tissue overload and flare-ups. Exercise should be challenging but within tolerance—this “therapeutic window” ensures adaptation without harm. Focusing only on gluteal strength is also problematic. Ignoring hip flexor tightness, core weakness, or movement dysfunction may miss underlying causes. A whole-body approach is essential. Returning too early to aggravating activities can reverse progress. A structured, criteria-based progression—rather than just symptom-based—is crucial to prevent reinjury and support lasting recovery.
Role of Home Exercise Programs (HEPs)
Home exercise programs (HEPs) extend the benefits of in-clinic therapy and support long-term recovery. HEPs should be tailored, progressive, and updated regularly based on patient improvement and goals. Key components include stretching tight muscles, strengthening the gluteal complex, and retraining functional movements. Simplicity and clarity are essential—patients must perform exercises correctly and consistently. Support tools like written guides, videos, or apps help ensure adherence and proper form. Ongoing reassessment keeps the program effective, advancing from basic to more complex or sport-specific activities as recovery progresses.
How Does It Compare to Other Treatments?
Understanding the relative effectiveness, risks, and benefits of shockwave therapy compared to alternative treatment options enables informed decision-making and appropriate treatment selection for individual patients.
Corticosteroid Injections
Corticosteroid injections provide quick pain relief by suppressing inflammation but may impair long-term tendon health. Studies show that while these injections reduce symptoms quickly, pain often returns within 3–6 months. Shockwave therapy, in contrast, promotes tissue healing and offers more lasting benefits. Unlike steroids, it stimulates regeneration rather than merely suppressing inflammation. Repeated corticosteroid use increases the risk of tendon weakening or rupture. Shockwave therapy has a much safer side-effect profile, typically limited to temporary discomfort or mild skin irritation. Due to these risks and limited durability, corticosteroids are falling out of favor for long-term tendinopathy management.
Platelet-Rich Plasma (PRP) Injections
PRP injections use a patient’s own platelets to deliver growth factors to the tendon. Like shockwave therapy, PRP promotes healing rather than just symptom relief. Some studies show comparable outcomes between PRP and shockwave therapy. However, shockwave therapy is non-invasive, less costly, and avoids injection-related risks. Combining PRP with shockwave therapy may enhance results in severe or resistant cases. Yet, due to its simplicity and repeatability, patients often prefer shockwave therapy over PRP, which is limited by cost and injection discomfort.
Surgical Interventions
Surgery is a last resort for gluteal tendinopathy when conservative options fail. Procedures may involve tendon debridement, bursectomy, or tendon repair. Surgical success rates vary (60–90%) and carry risks like infection, nerve damage, and long recovery (3–6 months). In contrast, shockwave therapy is low-risk, requires no downtime, and can allow patients to maintain daily activities during treatment. Many patients eligible for surgery can avoid it by using shockwave therapy. It’s also more cost-effective than surgery when factoring in hospital fees, anesthesia, and rehab.
Practical Considerations and FAQs
Understanding the practical aspects of shockwave therapy helps patients and healthcare providers make informed decisions about treatment implementation, set appropriate expectations, and optimize outcomes through proper preparation and post-treatment care.
Is Shockwave Therapy Painful?
Pain during shockwave therapy varies by patient, depending on tolerance, treatment settings, and the area treated. Most report a deep, pulsing sensation that’s uncomfortable but tolerable. Discomfort is typically strongest in the first few minutes and lessens as the session progresses, partly due to the therapy’s analgesic effects. To enhance comfort, clinicians often start at lower intensities and gradually increase energy. Modern devices offer adaptable applicators and protocols for individualized comfort. After treatment, soreness similar to post-exercise fatigue may occur, usually resolving in 24–48 hours. Some patients may experience a temporary symptom flare in the first week, which is normal and indicates tissue healing.
Considerations for Age-Related Tendon Degeneration
Aging tendons heal more slowly due to reduced collagen, blood supply, and elasticity. These changes impact treatment outcomes and require careful planning for older adults. Despite these challenges, shockwave therapy remains effective with modified protocols. Lower energy levels may be used initially, with gradual progression. More sessions may be needed to achieve results. Medical conditions like diabetes or cardiovascular disease and medications (e.g., anticoagulants) must be considered. A tailored rehabilitation plan is essential, focusing on strength, balance, and biomechanical correction to support tendon healing and prevent recurrence in aging populations.
Can I Resume Activity During Treatment?
Patients should avoid high-impact or aggravating activities (e.g., running, prolonged walking) during shockwave therapy but complete rest isn’t necessary. Low-impact options like swimming or cycling are typically safe if symptoms aren’t worsened. A gradual return to normal activity is recommended after therapy ends—starting 2–4 weeks post-treatment, guided by pain, functional progress, and imaging if needed. Work-related activity should be evaluated individually. Some patients continue working with adjustments, while others may need short-term restrictions. Communication with employers or occupational health services can support safe work continuation.
Are There Any Contraindications or Side Effects?
Shockwave therapy is generally safe, but contraindications exist. Absolute contraindications include pregnancy, malignancy in the treatment area, and proximity to pacemakers or implants. Bleeding disorders, infection, and anticoagulants are relative contraindications and need individualized assessment. Common side effects—such as mild bruising, redness, or swelling—resolve within a few days. Some patients experience a temporary symptom flare, which reflects a healing response. Rare risks include nerve irritation or tissue injury from excessive energy. These can be avoided through proper technique, equipment settings, and skilled clinicians.
Insurance Coverage and Cost Considerations
Shockwave therapy coverage varies. While some insurers cover it for conditions like plantar fasciitis or tennis elbow, coverage for gluteal tendinopathy may require prior authorization or may not be available. Despite upfront costs, shockwave therapy may reduce long-term expenses by avoiding surgery, medications, and lost work time. Some clinics offer packages or payment plans for those paying out-of-pocket. Considering both direct and indirect costs—like productivity loss or reduced quality of life—shockwave therapy often proves cost-effective over time.
Summary: A Powerful Option for Gluteal Tendinopathy Relief
Shockwave therapy has emerged as an effective, non-invasive treatment for gluteal tendinopathy, especially in cases unresponsive to conservative care. It promotes tendon healing through mechanical and biological mechanisms, offering pain relief and functional improvement with minimal risk. Optimal outcomes depend on proper timing—typically after 6–12 weeks of failed rehabilitation—and careful patient selection. Integration with a structured rehabilitation program enhances results, with home exercises playing a key role in long-term success. Compared to corticosteroid or PRP injections, shockwave therapy offers durable benefits without invasive procedures or injection-related risks. In many cases, it can help patients avoid surgery altogether. Its safety, growing clinical evidence, and favorable cost profile make it a powerful and accessible option for managing chronic lateral hip pain. When used judiciously and as part of a comprehensive treatment plan, shockwave therapy can significantly improve quality of life for patients suffering from gluteal tendinopathy.
References
- Shockwave Therapy for Tendinopathy
- How Shockwave Therapy Defeats Tendinopathy
- Long-Term Efficacy of Combined Focused and Radial Extracorporeal Shockwave Therapy for Gluteus Medius Tendon Pathology: A Pilot Study
- Long-term outcome of low-energy extracorporeal shockwave therapy on gluteal tendinopathy documented by magnetic resonance imaging
