Navicular syndrome remains one of the most challenging conditions affecting equine athletes, often leading to career-ending lameness if not properly managed. As veterinary medicine advances, shockwave therapy has emerged as a promising non-invasive treatment modality that addresses the complex pathophysiology underlying this debilitating condition. This comprehensive guide explores how extracorporeal shockwave therapy (ESWT) can revolutionize navicular syndrome management through targeted biomechanical intervention.
Understanding Navicular Syndrome: More Than Bone Deep
The complexity of navicular syndrome extends far beyond simple bone pathology, encompassing a multifaceted disorder that affects the entire navicular apparatus. Understanding this condition requires examining its etiology, progression patterns, and early manifestations to develop effective treatment strategies.
What Is Navicular Syndrome in Horses?
Navicular syndrome, also known as navicular disease or palmar heel pain syndrome, represents a degenerative condition affecting the navicular bone, navicular bursa, deep digital flexor tendon (DDFT), and associated ligamentous structures within the hoof capsule. The navicular bone serves as a fulcrum for the DDFT as it courses around the bone’s flexor surface, creating significant biomechanical stress during locomotion. This condition predominantly affects the forelimbs, particularly in horses with upright hoof conformation, and manifests as chronic progressive lameness characterized by shortened stride length and reluctance to engage the heel region during weight-bearing phases.
Common Causes and Progression
The etiopathogenesis of navicular syndrome involves multiple contributing factors that create a cascade of degenerative changes within the navicular apparatus. Poor hoof conformation, particularly upright pasterns and contracted heels, increases mechanical stress on the navicular bone and associated structures. Inadequate blood supply to the navicular bone, known as avascular necrosis, contributes to bone weakening and subsequent microfracture formation. The progression typically follows a predictable pattern: initial inflammation of the navicular bursa (bursitis), followed by adhesion formation between the DDFT and navicular bone, ultimately leading to bone sclerosis, cyst formation, and cortical erosion along the flexor surface.
Recognizing Early Signs of Chronic Hoof Pain
Early detection of navicular syndrome requires keen observation of subtle lameness patterns and behavioral changes that precede obvious clinical signs. Horses often demonstrate a characteristic “pottery” gait, landing toe-first to avoid heel contact and minimize navicular pressure. Intermittent lameness that worsens on hard surfaces or following periods of rest represents a hallmark feature of early disease progression. Additional indicators include shortened stride length, reluctance to turn in tight circles, and positive response to palmar digital nerve blocks. Behavioral changes such as reluctance to work, increased irritability during hoof handling, and altered resting postures where the affected limb is frequently pointed forward may indicate developing navicular pathology before lameness becomes apparent.
Shockwave Therapy for Navicular Syndrome: A Modern Approach
Shockwave therapy has revolutionized the treatment landscape for navicular syndrome by offering a non-invasive alternative to traditional surgical interventions. This therapeutic modality harnesses acoustic waves to stimulate healing processes at the cellular level, making it particularly well-suited for addressing the complex pathophysiology of navicular disease.
What Is Shockwave Therapy?
Extracorporeal shockwave therapy (ESWT) utilizes high-energy acoustic waves generated outside the body and focused on specific tissue targets to promote healing and pain reduction. These acoustic waves create mechanical stress within tissues, triggering a cascade of biological responses including neovascularization, cellular proliferation, and anti-inflammatory effects. The therapy operates through mechanotransduction, where mechanical energy is converted into biochemical signals that stimulate tissue repair mechanisms. ESWT has demonstrated efficacy in treating various musculoskeletal conditions by promoting osteoblast activity, enhancing collagen synthesis, and modulating pain perception through neuromodulation pathways. The non-invasive nature of ESWT makes it particularly attractive for treating conditions within the confined hoof capsule where surgical access is limited.
Focused vs Radial Shockwaves: Which Works for Hoof?
The selection between focused and radial shockwave modalities depends on the specific pathological targets within the navicular apparatus and treatment objectives. Focused shockwaves (F-ESWT) generate high-energy pulses that converge at a specific focal point, typically 2-8mm in diameter, allowing precise targeting of deep structures like the navicular bone and DDFT interface. This modality proves particularly effective for addressing bone pathology, including sclerosis and cyst formation, due to its ability to penetrate deep tissues with minimal energy dissipation. Radial shockwaves (R-ESWT) create pressure waves that spread radially from the applicator, affecting larger tissue volumes but with lower energy density. R-ESWT excels in treating superficial soft tissue conditions and may be preferred for addressing navicular bursa inflammation and surrounding fascial restrictions that contribute to biomechanical dysfunction.
How Shockwave Interacts with Hoof Structures
The interaction between shockwave energy and hoof structures creates a complex pattern of mechanical stimulation that influences healing processes throughout the navicular apparatus. The hoof capsule’s unique composition, consisting of keratinized horn wall, sole, and frog, creates acoustic impedance variations that affect shockwave propagation patterns. Energy transmission through the hoof wall depends on hydration status, horn quality, and structural integrity, requiring careful consideration of treatment parameters to ensure adequate energy delivery to target tissues. The navicular bone’s position within the hoof capsule, surrounded by synovial fluid and soft tissues, creates an ideal environment for shockwave-induced mechanotransduction. Acoustic waves stimulate osteoblast activity along the navicular bone’s surface while simultaneously promoting synovial fluid circulation and reducing inflammatory mediators within the navicular bursa.
Biological Mechanisms: How Healing Happens
The therapeutic efficacy of shockwave therapy in navicular syndrome stems from its ability to trigger multiple biological pathways that address the underlying pathophysiology of the condition. Understanding these mechanisms provides insight into optimal treatment protocols and expected outcomes.
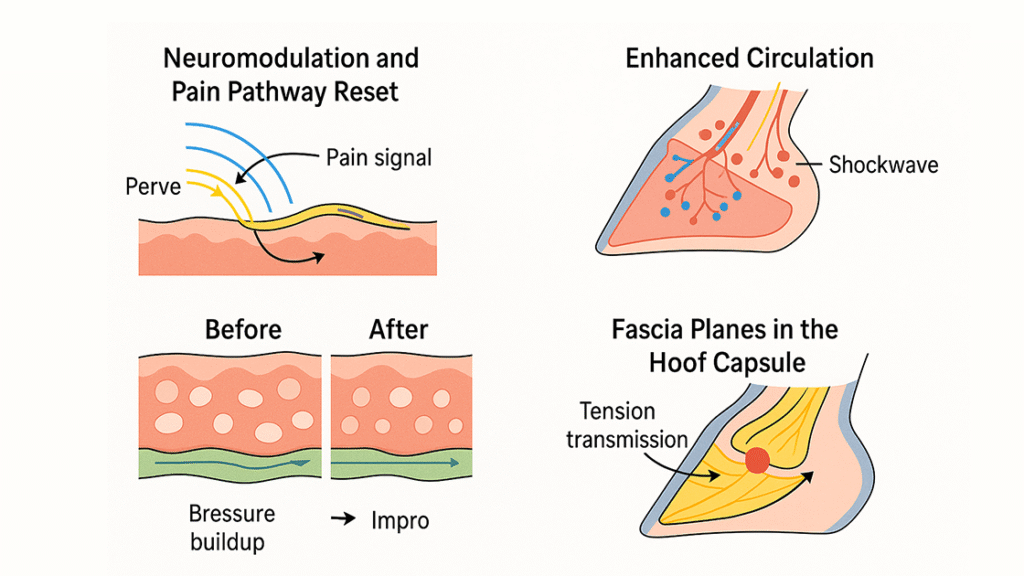
Neuromodulation and Pain Pathway Reset
Shockwave therapy exerts profound effects on nociceptive pathways, providing immediate and long-term pain relief through multiple neuromodulatory mechanisms. The gate control theory explains how shockwave-induced mechanical stimulation of large-diameter A-beta fibers can inhibit pain transmission through small-diameter C-fibers at the spinal cord level. Additionally, ESWT stimulates the release of endogenous opioids and substance P depletion, creating analgesic effects that persist beyond the immediate treatment period. Neuroplasticity changes occur within the dorsal horn of the spinal cord, where repeated shockwave treatments can reset aberrant pain processing patterns associated with chronic navicular pain. The hyperstimulation analgesia effect, where intense non-noxious stimulation blocks pain perception, provides immediate relief that allows horses to resume normal gait patterns and weight-bearing behaviors essential for continued healing.
Enhanced Circulation in the Navicular Region
Vascular compromise represents a critical factor in navicular syndrome pathogenesis, making the pro-angiogenic effects of shockwave therapy particularly relevant for treatment success. ESWT stimulates the release of vascular endothelial growth factor (VEGF), fibroblast growth factor (FGF), and other angiogenic mediators that promote new blood vessel formation within the navicular bone and surrounding tissues. Mechanotransduction pathways activated by shockwave energy trigger endothelial cell proliferation and migration, leading to improved microcirculation in previously hypoxic regions. The increased blood flow enhances nutrient delivery and waste product removal, creating an optimal environment for tissue repair. Doppler ultrasound studies have documented sustained improvements in navicular bone perfusion following ESWT treatment, correlating with clinical improvement and reduced lameness scores in affected horses.
Cellular Regeneration and Collagen Remodeling
The regenerative potential of shockwave therapy extends to both osseous and soft tissue components of the navicular apparatus through stimulation of cellular proliferation and extracellular matrix remodeling. Acoustic energy stimulates osteoblast activity and promotes new bone formation, particularly beneficial for addressing navicular bone sclerosis and cyst formation. Simultaneously, ESWT enhances fibroblast proliferation and collagen synthesis within the DDFT and associated ligamentous structures. The mechanical stress induced by shockwave treatment triggers the expression of growth factors including bone morphogenetic proteins (BMPs), transforming growth factor-beta (TGF-β), and insulin-like growth factor-1 (IGF-1). These factors promote tissue regeneration while simultaneously modulating inflammatory responses to prevent excessive scar tissue formation. The result is improved tissue quality and biomechanical function throughout the navicular apparatus.
Fascia, Flow, and Biomechanics: Hidden Influences in Recovery
The holistic approach to navicular syndrome treatment must consider the interconnected nature of fascial networks, lymphatic drainage, and biomechanical function within the equine limb. These often-overlooked factors significantly influence treatment outcomes and long-term soundness.
Fascia Planes in the Hoof Capsule and Their Role in Pain
The fascial architecture within the hoof capsule creates a complex network of interconnected tissue planes that significantly influence biomechanical function and pain perception in navicular syndrome. The digital cushion, composed of fibro-fatty tissue and elastic fibers, serves as a shock-absorbing structure that interfaces with the navicular apparatus during weight-bearing. Fascial restrictions within this region can create abnormal stress patterns that exacerbate navicular pathology by altering load distribution across the hoof. The deep digital flexor tendon is enveloped by fascial sheaths that facilitate smooth gliding motion around the navicular bone. Adhesions or fibrosis within these fascial planes can create mechanical restrictions that increase friction and inflammatory responses. Shockwave therapy’s ability to break down fascial adhesions and promote tissue remodeling makes it particularly effective for addressing these hidden contributors to navicular syndrome.
Lymphatic Clearance and Edema Reduction
Lymphatic drainage plays a crucial role in maintaining tissue homeostasis within the hoof capsule, and impaired lymphatic function contributes to the chronic inflammatory state characteristic of navicular syndrome. The confined nature of the hoof capsule creates challenges for lymphatic drainage, particularly when inflammatory processes increase tissue volume and pressure. ESWT enhances lymphatic flow through mechanical stimulation of lymphatic vessels and surrounding tissues, promoting the clearance of inflammatory mediators and metabolic waste products. The pulsatile nature of shockwave energy creates a pumping effect that facilitates lymphatic propulsion, while simultaneously reducing tissue edema through improved microcirculation. This enhanced lymphatic clearance contributes to the anti-inflammatory effects of ESWT and helps maintain the optimal tissue environment necessary for healing processes to occur effectively within the navicular apparatus.
Dynamic Diagnostics: Using Movement + Shockwave for Custom Targeting
Advanced diagnostic techniques that combine movement analysis with shockwave therapy enable precise treatment targeting and objective assessment of therapeutic outcomes. This personalized approach optimizes treatment protocols based on individual biomechanical patterns and pathological presentations.
Pressure Mapping and Real-Time Gait Feedback
Pressure mapping technology provides invaluable insights into load distribution patterns within the hoof, enabling clinicians to identify specific regions of abnormal stress that contribute to navicular syndrome progression. Digital pressure plates and in-shoe pressure sensors can detect subtle changes in weight-bearing patterns that may not be apparent through traditional lameness evaluation methods. Real-time gait analysis systems utilize high-speed cameras and motion sensors to quantify stride characteristics, joint angles, and temporal gait parameters with unprecedented precision. This objective data allows for customized shockwave treatment protocols that target specific biomechanical dysfunction patterns. Integration of pressure mapping with shockwave therapy enables immediate assessment of treatment effects, allowing for real-time protocol adjustments to optimize therapeutic outcomes. The combination of these technologies provides a comprehensive understanding of how shockwave therapy influences biomechanical function and guides evidence-based treatment decisions.
Functional Ultrasound Before & After Shockwave
Functional ultrasound imaging represents a revolutionary diagnostic tool that enables dynamic assessment of navicular apparatus structures during weight-bearing and movement. Unlike traditional static ultrasound, functional imaging captures real-time changes in tissue architecture, blood flow, and structural relationships during locomotion. Pre-treatment functional ultrasound establishes baseline measurements of navicular bone morphology, DDFT integrity, and synovial fluid characteristics that guide treatment planning. Post-treatment imaging documents objective improvements in tissue quality, vascular perfusion, and structural integrity that correlate with clinical improvement. Doppler ultrasound assessment of navicular bone blood flow provides quantitative measurements of ESWT’s vascular effects, enabling optimization of treatment intervals and energy settings. The integration of functional ultrasound with shockwave therapy protocols creates a feedback loop that ensures treatment precision while providing objective evidence of therapeutic efficacy for both clinicians and horse owners.
Bioindividual Protocols: Shockwave Based on the Horse’s Internal Clock
Personalized medicine approaches in equine healthcare recognize that individual horses respond differently to therapeutic interventions based on their unique physiological characteristics and circadian rhythms. This bioindividual approach to shockwave therapy optimizes treatment outcomes by aligning therapeutic interventions with each horse’s natural healing processes.
Circadian Healing Windows in Equine Recovery
Circadian rhythms significantly influence cellular repair mechanisms, inflammatory responses, and pain perception in horses, making treatment timing a critical factor in shockwave therapy success. Cortisol levels naturally fluctuate throughout the day, with peak concentrations occurring in early morning hours, influencing the body’s inflammatory response and healing capacity. Growth hormone release follows a circadian pattern, with maximum secretion occurring during deep sleep phases, making evening treatments potentially more effective for promoting tissue regeneration. Melatonin production, which begins at sunset, possesses anti-inflammatory and antioxidant properties that may enhance shockwave therapy outcomes when treatments are timed to coincide with natural melatonin elevation. Temperature regulation and metabolic activity also follow circadian patterns that influence tissue responsiveness to mechanical stimulation. Understanding these natural rhythms allows clinicians to schedule shockwave treatments during optimal healing windows, potentially improving therapeutic efficacy while minimizing adverse effects.
HRV (Heart Rate Variability) as a Readiness Marker
Heart rate variability serves as a valuable biomarker for assessing autonomic nervous system function and physiological readiness for therapeutic intervention in horses with navicular syndrome. HRV analysis provides insights into the balance between sympathetic and parasympathetic nervous system activity, which directly influences inflammatory responses, pain perception, and tissue healing capacity. Horses experiencing chronic pain often demonstrate reduced HRV, indicating autonomic dysfunction that may impair healing processes. Pre-treatment HRV assessment helps identify optimal treatment timing by ensuring the horse’s physiological state is conducive to positive therapeutic outcomes. Post-treatment HRV monitoring provides objective evidence of treatment efficacy, as improvements in autonomic function often correlate with reduced pain and enhanced well-being. Integration of HRV monitoring with shockwave therapy protocols enables personalized treatment schedules that respect each horse’s individual physiological state and optimize therapeutic outcomes through precise timing of interventions.

Shifting the Owner’s Mindset: From ‘Fix-It’ to ‘Re-Tune It’
Successful navicular syndrome management requires a fundamental shift in how horse owners conceptualize lameness and treatment goals. This paradigm change from reactive crisis management to proactive maintenance and optimization creates better outcomes and improved quality of life for affected horses.
Rethinking Maintenance: Shockwave for Longevity, Not Just Crisis
The traditional approach to navicular syndrome treatment often focuses on crisis intervention when lameness becomes severe, missing opportunities for preventive care that could maintain soundness and prevent progression. Proactive shockwave therapy protocols, implemented before obvious lameness develops, can address subclinical pathology and maintain optimal tissue health throughout the horse’s career. Regular maintenance treatments help preserve navicular bone integrity, maintain synovial fluid quality, and prevent the development of compensatory biomechanical patterns that accelerate degenerative changes. This preventive approach recognizes that navicular syndrome represents a chronic progressive condition that benefits from consistent management rather than episodic intervention. Owner education about the benefits of maintenance protocols helps establish realistic expectations about treatment outcomes and promotes long-term commitment to comprehensive care strategies that optimize horse welfare and performance longevity.
Owner Education: Why ‘Lameness’ Starts Before the Limp
Educating horse owners about the subtle early signs of navicular syndrome empowers them to seek intervention before irreversible damage occurs, significantly improving treatment outcomes and prognosis. Many owners associate lameness only with obvious gait abnormalities, missing the subtle behavioral and performance changes that indicate developing pathology. Understanding that pain perception occurs before visible lameness helps owners recognize when their horses may benefit from diagnostic evaluation and early intervention. Changes in attitude, work ethic, or performance often precede obvious lameness and represent opportunities for early treatment that can prevent disease progression. Owner education about biomechanical risk factors, proper hoof care, and the importance of regular veterinary evaluation creates a partnership approach to navicular syndrome management. This collaborative relationship between owners and veterinarians ensures that treatment decisions are based on comprehensive understanding of the condition and realistic expectations about outcomes.
Do Horses Behave Differently After Chronic Pain Is Reduced?
Horses treated successfully for navicular syndrome often show marked behavioral changes, signaling improved comfort and limb function. Common signs include increased willingness to back up, turn sharply, or work on uneven ground—activities they previously avoided. Horses may become more engaged during training, with a better attitude and work ethic. Pain relief often improves sleep, allowing horses to lie down more comfortably and rise with ease. Socially, they may appear more confident and active within the herd. These subtle yet meaningful changes offer valuable insights into treatment effectiveness and help owners adjust training and care strategies accordingly.
What’s Next: Combining Shockwave with Neuromodulation, PEMF, or AI Gait Monitoring
The future of navicular syndrome treatment lies in combining shockwave therapy with emerging technologies for a more targeted and effective approach. Neuromodulation tools like TENS may enhance pain relief by supporting long-term neural recovery. PEMF therapy adds another layer of cellular repair through electromagnetic stimulation, working synergistically with shockwave. Meanwhile, AI-powered gait analysis offers real-time monitoring of subtle movement changes, allowing for personalized treatment adjustments. Wearable sensors enable 24/7 tracking of activity and early detection of setbacks. Together, these innovations bring a more precise, proactive, and holistic way to manage navicular syndrome—moving beyond symptom control to true functional recovery.
FAQs About Navicular Syndrome and Shockwave Therapy
Yes. Beyond numbing pain, focused shockwave may influence central sensitization—a condition where the nervous system becomes hypersensitive. Research suggests it could help “retrain” the brain’s response to chronic hoof pain, contributing to longer-term relief.
AI systems detect micro-lameness patterns invisible to the human eye. This enables real-time protocol adjustments, ensures treatment is hitting the mark, and may prevent over- or under-treatment of the affected limb.
Absolutely. PEMF (Pulsed Electromagnetic Field therapy) promotes cellular regeneration and circulation. When used alongside shockwave, the two modalities may work synergistically to reduce inflammation and support tissue healing through complementary mechanisms.
Innovative tools like pressure mapping, heart rate variability (HRV), and movement sensors can track subtle physiological responses. These markers often shift before external lameness improves, giving you a head start on evaluating effectiveness.
Emerging research in circadian biology suggests that equine tissue repair and inflammation cycles fluctuate with time of day. Timing shockwave sessions to these “healing windows” could enhance effectiveness—though this approach is still experimental.
Yes. Many progressive clinicians now use low-frequency maintenance shockwave for chronic cases or high-performance horses. This proactive use may delay structural degeneration, reduce flare-ups, and support ongoing biomechanical balance.
References
- What is shockwave therapy for horses?
- Veterinarian’s Perspective of Shockwave Therapy for Horses
- Why Every Horse Owner Should Consider Shockwave Therapy
- Boost Your Horse’s Wellness: Shockwave Therapy for Equine Health
- Sustainable treatment success of an Os naviculare syndrome using conservative measures, infiltration therapy, and shock waves
Systematic Review of Complementary and Alternative Veterinary Medicine in Sport and Companion Animals: Extracorporeal Shockwave Therapy
