Введение
Morton’s neuroma is one of the most frequent causes of forefoot pain, particularly in middle-aged adults. Many patients first notice discomfort when walking long distances, exercising, or wearing tight shoes. While some dismiss it as a temporary irritation, the condition can progress and significantly impair daily life. To fully understand why podiatrists increasingly recommend shockwave therapy, it is essential to examine Morton’s neuroma, traditional treatment limitations, and the role of modern non-surgical care. The first step in this journey is gaining a clear understanding of what Morton’s neuroma is and why it occurs. By exploring its definition and medical basis, patients can better appreciate how the condition develops and why timely intervention matters.
Overview of Morton’s Neuroma as a Common Foot Condition
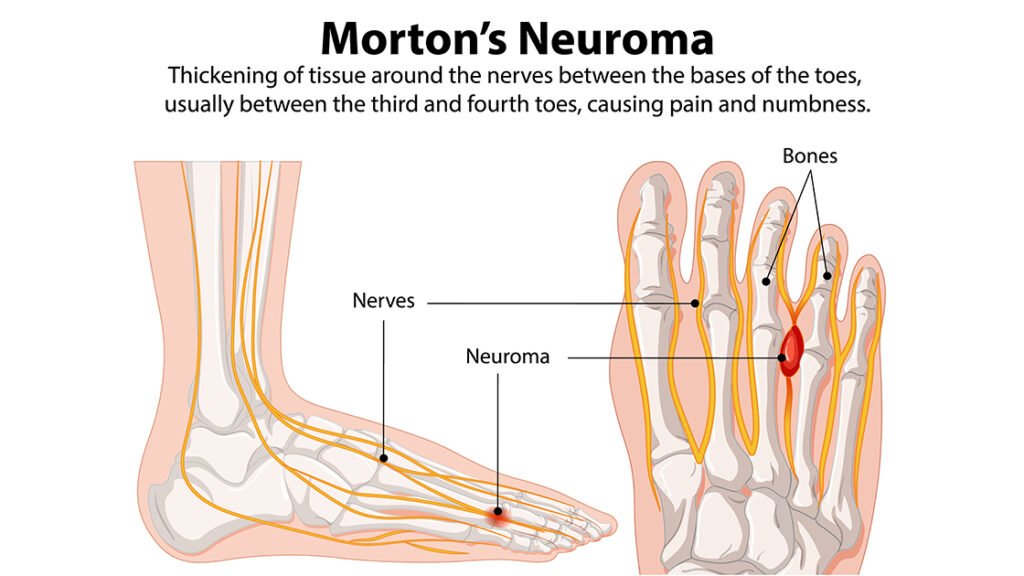
Morton’s neuroma is a painful foot disorder caused by thickening of the tissue around one of the nerves leading to the toes, usually between the third and fourth metatarsal heads. The condition is sometimes referred to as “interdigital neuroma” or “perineural fibrosis,” highlighting its basis in nerve irritation and tissue degeneration rather than being a true tumor. Patients often describe the sensation as walking with a small stone in their shoe, accompanied by sharp, burning pain radiating into the toes. This pain worsens with tight footwear or prolonged activity. Morton’s neuroma is more prevalent in women, often linked to narrow or high-heeled shoes, though athletes and people with abnormal foot biomechanics are also at higher risk. Because the condition can worsen over time, early diagnosis and treatment are crucial to prevent nerve damage and restore mobility before symptoms become debilitating.
The Challenges of Traditional Treatments (Injections, Orthotics, Surgery)
- Footwear modifications and custom orthotics aim to reduce mechanical pressure on the affected nerve, offering temporary relief.
- Corticosteroid injections target inflammation and swelling around the nerve to alleviate pain.
- Repeated injections may cause tissue weakening or symptom recurrence over time.
- Surgical excision of the affected nerve can provide more definitive relief but carries risks such as infection or numbness.
- Surgery requires anesthesia and often weeks of restricted activity, disrupting daily life.
Why Shockwave Therapy Is Emerging as a Preferred Non-Surgical Option
Ударно-волновая терапия, also known as Extracorporeal Shockwave Therapy (ESWT), has gained recognition among podiatrists as a highly effective, non-invasive alternative for treating Morton’s neuroma. The treatment delivers focused acoustic waves to the affected nerve and surrounding tissue, stimulating natural healing processes, improving blood circulation, and reducing nerve irritation. Unlike corticosteroid injections or surgery, shockwave therapy minimizes the risk of tissue damage and infection, requires no anesthesia, and allows patients to resume normal activities shortly after treatment. Clinical studies indicate that ESWT not only alleviates pain but also promotes tissue regeneration, addressing the root cause of neuroma discomfort. Its combination of safety, efficacy, and convenience has made it a preferred choice for patients seeking long-term relief from forefoot neuropathic pain.
Understanding Morton’s Neuroma
After examining why shockwave therapy is becoming a preferred treatment, it is essential to understand the condition it addresses. A detailed understanding of Morton’s neuroma—including its definition, underlying mechanisms, causes, symptoms, and daily impact—helps patients recognize the importance of early intervention. By understanding the pathophysiology and risk factors, individuals can make informed decisions about treatment options, preventive strategies, and lifestyle adjustments that complement medical therapies.
What Is Morton’s Neuroma? Definition and Pathophysiology
Morton’s neuroma is classified as a perineural fibrosis of the common plantar digital nerve, most commonly located between the third and fourth toes. It is not a true tumor but a benign enlargement of the nerve caused by chronic compression and irritation. Repetitive mechanical stress leads to demyelination, nerve fiber degeneration, and fibrotic tissue proliferation, which compresses the nerve further. This results in neuropathic pain characterized by burning sensations, tingling, and occasional numbness. Over time, if left untreated, the nerve may become hypersensitive, and symptoms can intensify, interfering with normal gait and daily activities. Understanding this pathophysiology underscores why treatments addressing both nerve irritation and tissue regeneration—like shockwave therapy—are increasingly favored by podiatrists.
Common Causes and Risk Factors (Footwear, Overuse, Biomechanics)
- Improper footwear, such as high heels or narrow-toed shoes, compresses the metatarsal heads and increases pressure on the interdigital nerve.
- Repetitive stress from running, dancing, or jumping sports can exacerbate nerve irritation.
- Anatomical variations like flat feet, bunions, or hammertoes alter forefoot biomechanics, increasing neuroma risk.
- Women are disproportionately affected due to footwear choices and anatomical predispositions.
Symptoms of Morton’s Neuroma: Burning Pain, Numbness, Tingling
- Sharp or burning pain in the forefoot, often radiating toward the toes, is a hallmark symptom.
- Tingling, numbness, or the sensation of a small object under the foot may occur.
- Symptoms typically worsen with walking, running, or wearing tight shoes.
- Pain often improves with rest or removing shoes.
- In severe cases, pain can become constant, affecting daily tasks and limiting mobility.
How Morton’s Neuroma Impacts Daily Life and Mobility
- Morton’s neuroma can limit mobility and cause chronic discomfort, disrupting daily life.
- Individuals may avoid physical activities or alter their gait to reduce pain.
- Shifting weight to compensate can lead to secondary issues, such as knee, hip, or lower back strain.
- Chronic neuropathic pain can affect mental health, causing frustration, stress, and lower quality of life.
- Even simple tasks like standing for long periods, walking in tight shoes, or participating in sports can become challenging.
Traditional Treatments for Morton’s Neuroma
Before exploring innovative options like shockwave therapy, it is important to review conventional treatments for Morton’s neuroma. Traditional approaches focus on reducing nerve irritation and alleviating pain but often come with limitations. Understanding these methods—ranging from conservative management to surgical interventions—helps patients recognize why newer, non-invasive treatments are gaining favor. Evaluating benefits, risks, and limitations is essential for informed decision-making and effective long-term foot health management.
Conservative Management: Footwear Changes, Orthotics, Physical Therapy
Conservative management is typically the first line of treatment for Morton’s neuroma. Footwear modifications, such as shoes with a wider toe box and lower heels, reduce pressure on the affected nerve. Custom orthotic inserts redistribute weight across the foot to minimize metatarsal stress and alleviate discomfort. Physical therapy can further improve foot mechanics through stretching, strengthening, and soft tissue mobilization, promoting better gait patterns and reducing nerve irritation. While these strategies often provide temporary symptom relief, they rarely reverse underlying nerve fibrosis. Nevertheless, conservative management is essential for patients seeking non-invasive measures, for early-stage neuromas, or for those who are not candidates for injections or surgery.
Corticosteroid Injections and Their Limitations
Corticosteroid injections are frequently used to reduce inflammation and swelling around the affected interdigital nerve. They provide short-term pain relief by decreasing immune-mediated tissue responses and improving local circulation. However, repeated injections carry risks, including tissue atrophy, nerve damage, or fat pad degeneration. Additionally, the relief is often temporary, with symptoms potentially returning within weeks to months. These limitations make injections a palliative rather than curative treatment. Patients may also experience discomfort during the procedure and require multiple sessions to achieve modest improvement, emphasizing the need for more sustainable, non-invasive alternatives like shockwave therapy.
Surgical Interventions: Risks, Recovery, and Recurrence
Surgery, typically neurectomy of the affected interdigital nerve, is considered when conservative and injection-based therapies fail. While surgery can provide definitive pain relief, it carries several inherent risks. Patients may face infection, wound healing complications, scar formation, or postoperative numbness in the toes. Recovery often requires several weeks of limited weight-bearing and activity restrictions. Furthermore, neuroma recurrence can occur in a subset of patients, sometimes necessitating revision surgery. Given these factors, many individuals are hesitant to pursue surgery unless symptoms are severe or unresponsive to other interventions, highlighting the value of non-surgical therapies that address pain with lower risk and downtime.
Why Patients Seek Alternatives to Surgery and Drugs
Many patients with Morton’s neuroma actively seek alternatives due to the drawbacks of traditional interventions. Fear of surgical complications, extended recovery times, and post-operative numbness often motivate patients to explore non-invasive solutions. Similarly, reliance on medications such as corticosteroids or NSAIDs carries risks of systemic side effects, including gastrointestinal, renal, or cardiovascular complications with long-term use. Non-invasive therapies that reduce pain, improve mobility, and promote tissue healing without pharmacologic or surgical risks are increasingly attractive. Shockwave therapy, with its demonstrated efficacy and minimal downtime, has emerged as a preferred option for patients who desire sustainable relief while avoiding conventional treatment drawbacks.
Introduction to Shockwave Therapy (ESWT)
After examining conventional treatments, it is clear that many patients seek safer, non-invasive alternatives for Morton’s neuroma. Shockwave therapy, also known as Extracorporeal Shockwave Therapy (ESWT), has emerged as a promising solution. By using high-energy acoustic waves targeted at the affected nerve and surrounding tissues, ESWT promotes natural healing mechanisms while minimizing downtime. Understanding the technology, mechanism, and clinical safety profile helps patients and clinicians appreciate why ESWT is increasingly recommended in podiatric care.
What Is Shockwave Therapy? Medical Definition and Technology
Shockwave therapy is a non-invasive medical procedure that uses high-energy acoustic waves to stimulate tissue repair and reduce pain. The device generates focused pulses that penetrate the skin and underlying structures without the need for incisions or anesthesia. Modern ESWT devices are calibrated to deliver specific energy levels and frequencies suitable for treating neuromas in the forefoot. The technology enables precise targeting of the interdigital nerve and surrounding fibrotic tissue, promoting tissue regeneration while avoiding damage to healthy structures. Clinically, ESWT is distinguished from low-energy therapies by its higher intensity, which is sufficient to induce controlled microtrauma that triggers reparative processes. Its versatility allows treatment of various musculoskeletal and neuropathic conditions, making it a valuable tool in podiatry.
Mechanism of Action: How Shockwaves Stimulate Healing in Nerve Tissue
Shockwave therapy works through a combination of mechanical and biological mechanisms. Acoustic waves induce microtrauma in fibrotic tissue, stimulating localized angiogenesis and enhancing blood circulation around the affected nerve. This improved perfusion supports oxygen delivery and waste removal, critical for nerve recovery. Additionally, ESWT modulates nerve excitability, reducing abnormal pain signaling and hyperalgesia. The therapy also triggers mechanotransduction pathways that activate fibroblasts and Schwann cells, promoting extracellular matrix remodeling and nerve regeneration. Repetitive sessions enhance collagen synthesis, break down scar tissue, and restore normal nerve architecture. By addressing both structural and neurological components of Morton’s neuroma, ESWT provides more comprehensive pain relief than therapies that solely mask symptoms.
Safety Profile and Evidence-Based Effectiveness for Foot Pain
Shockwave therapy is generally safe when administered by trained clinicians. Adverse events are rare and usually limited to mild, transient swelling, redness, or discomfort at the treatment site. No anesthesia or incisions are required, minimizing infection risk and recovery time. Clinical studies demonstrate significant pain reduction and improved function in patients with Morton’s neuroma after 3–5 weekly sessions. Research shows that over 70% of patients report meaningful symptom relief, with low recurrence rates. Evidence-based guidelines emphasize proper patient selection, appropriate energy dosing, and adherence to standardized treatment protocols to optimize outcomes. Overall, ESWT provides an effective, minimally invasive option for chronic neuropathic foot pain.
Benefits of Shockwave Therapy for Morton’s Neuroma
Transitioning from conventional treatments, shockwave therapy offers a suite of clinical advantages. By targeting the underlying pathology rather than only suppressing pain, ESWT addresses nerve irritation, fibrosis, and inflammation. Patients benefit from non-invasive therapy, minimal side effects, and improved long-term outcomes. Understanding these benefits underscores why podiatrists increasingly recommend ESWT as a frontline or adjunctive treatment for Morton’s neuroma.
Non-Invasive Alternative to Surgery and Injections
Shockwave therapy provides a non-surgical approach, avoiding the risks associated with neurectomy or repeated corticosteroid injections. Patients experience effective pain relief without anesthesia, incisions, or prolonged recovery. The non-invasive nature allows treatment in outpatient settings, often while maintaining daily activities. By eliminating the surgical risk of nerve damage, infection, and post-operative numbness, ESWT offers a safer alternative for individuals who prefer conservative care or have contraindications to surgery. This makes it particularly appealing for patients seeking long-term, functional improvements in foot health.
Reduction in Pain and Inflammation Without Medications
ESWT alleviates pain through modulation of nerve excitability and reduction of local inflammation. Acoustic waves stimulate blood flow and decrease pro-inflammatory cytokines around the affected nerve. Unlike oral medications, such as NSAIDs or corticosteroids, ESWT avoids systemic side effects, including gastrointestinal, renal, or cardiovascular risks. The localized, mechanical nature of treatment directly targets the source of pain rather than merely masking symptoms, resulting in faster and more durable relief. Patients often notice significant improvements within 2–3 sessions, enhancing quality of life without pharmacological dependence.
Stimulation of Tissue Regeneration and Nerve Healing
One of the key advantages of ESWT is its ability to promote regenerative processes. Mechanical stimulation activates fibroblasts, Schwann cells, and angiogenesis, encouraging repair of fibrotic tissue and the affected interdigital nerve. Collagen remodeling and microvascular improvements restore nerve architecture and functionality. Over several weeks, tissue regeneration reduces nerve compression and hyperalgesia, providing sustained analgesia. Unlike palliative treatments, this regenerative effect addresses the underlying cause of Morton’s neuroma, improving long-term outcomes and minimizing recurrence risk.
Improved Foot Function, Mobility, and Quality of Life
By reducing pain and restoring tissue integrity, ESWT improves overall foot biomechanics and mobility. Patients experience less discomfort when walking, running, or performing daily tasks, enabling a return to normal activities. Enhanced foot function also reduces compensatory gait changes that can lead to secondary joint or musculoskeletal issues. Clinically, improved mobility correlates with higher patient satisfaction, better adherence to exercise regimens, and overall enhancement of physical and psychological well-being.
Long-Lasting Relief with Minimal Downtime
ESWT provides durable pain relief, often lasting several months to a year, depending on neuroma severity and patient adherence to post-treatment care. Sessions typically require no downtime, allowing patients to resume daily activities immediately. The combination of long-lasting results and minimal disruption makes ESWT an attractive option compared to surgery or repeated injections, which involve recovery periods and higher complication risks. Patients benefit from sustainable symptom management, enhanced functionality, and a low-risk profile.
Клинические данные в поддержку ударно-волновой терапии
Understanding the clinical evidence behind shockwave therapy is crucial for patients and practitioners. Evidence from peer-reviewed studies, comparative analyses, and real-world case reports demonstrates its efficacy for Morton’s neuroma. Evaluating research outcomes alongside podiatric experience helps establish confidence in ESWT as a viable, non-invasive alternative to injections and surgery. Reviewing success rates, long-term effects, and recurrence prevention provides a comprehensive view of why podiatrists increasingly recommend this therapy.
Research Studies on Shockwave Therapy for Morton’s Neuroma
Multiple studies have examined ESWT for Morton’s neuroma, consistently showing significant reductions in pain and functional improvement. Randomized controlled trials reveal that patients receiving focused shockwave therapy experience decreased neuropathic pain scores, improved walking tolerance, and enhanced quality of life. Mechanistically, studies confirm increased local microcirculation, reduced nerve compression, and regenerative tissue responses. Clinical trials typically involve 3–5 weekly sessions, and follow-up evaluations demonstrate sustained analgesic effects over 6–12 months. Research also indicates that ESWT may reduce reliance on medications and delay or prevent the need for surgery. Collectively, these studies validate ESWT as a reliable, evidence-based approach for managing chronic interdigital neuropathic pain.
Success Rates Compared to Cortisone and Surgery
Comparative studies suggest that ESWT offers competitive, and often superior, outcomes relative to corticosteroid injections. While injections provide temporary relief, shockwave therapy promotes longer-lasting analgesia by addressing underlying nerve fibrosis and tissue degeneration. In surgical cohorts, neurectomy provides definitive pain relief but carries higher risks of complications, such as postoperative numbness, infection, or scar formation. ESWT success rates generally range between 70–85%, with low recurrence and minimal adverse effects, making it a safer alternative for patients seeking effective, non-invasive treatment. Podiatrists often recommend ESWT prior to considering surgical intervention to optimize patient safety and satisfaction.

Podiatrists’ Clinical Experience and Patient Case Studies
Podiatrists report high satisfaction rates among patients treated with ESWT for Morton’s neuroma. Case studies highlight rapid pain reduction, improved walking patterns, and minimal downtime. Clinicians note that early intervention leads to better outcomes, particularly when combined with footwear modifications or orthotics. Documented cases show functional recovery within weeks, with patients returning to sports and daily activities without pharmacologic support. These real-world experiences reinforce clinical trial findings, providing practical evidence that supports ESWT as a primary or adjunctive therapy in neuropathic foot care.
Long-Term Outcomes and Recurrence Prevention
Long-term follow-up studies indicate that shockwave therapy can reduce neuroma recurrence by promoting structural repair of the interdigital nerve and surrounding tissue. Sustained improvements in pain scores, foot function, and quality of life are observed for up to 12 months post-treatment. Repeated or maintenance sessions may further enhance durability, especially in patients with ongoing biomechanical stress. By addressing both inflammatory and fibrotic components of the neuroma, ESWT minimizes the risk of symptom relapse compared to conservative management or pharmacologic therapies alone, offering a comprehensive, long-term solution for neuropathic forefoot pain.
What to Expect During Shockwave Therapy Sessions
For patients considering ESWT, understanding what occurs during treatment reduces anxiety and sets realistic expectations. Proper patient preparation, procedural steps, treatment sensations, and recovery timelines are all important considerations. Educating patients about these factors improves compliance and enhances the perceived efficacy of therapy. Knowing how each session works and the anticipated outcomes helps patients feel confident and engaged in their own care.
How the Procedure Works Step by Step
During a shockwave therapy session, the podiatrist identifies the neuroma location using palpation or imaging guidance. The treatment area is marked, and a coupling gel is applied to optimize acoustic wave transmission. The ESWT device delivers high-energy shockwaves directly to the affected nerve and surrounding tissue. Each pulse stimulates microtrauma, enhancing circulation, nerve regeneration, and fibroblast activation. The procedure is non-invasive and performed in an outpatient setting. Patients may undergo several treatment zones depending on symptom distribution, ensuring comprehensive coverage of the interdigital nerve and associated fibrotic tissue.
Typical Treatment Duration, Frequency, and Protocols
A standard ESWT regimen for Morton’s neuroma consists of 3–5 weekly sessions, each lasting approximately 10–15 minutes. The number of shockwaves per session is typically calibrated between 1,000–2,500 pulses at a frequency of 4–6 Hz, depending on device settings and patient tolerance. Clinicians may adjust energy flux density to balance therapeutic efficacy with comfort. Full treatment protocols are designed to maximize tissue regeneration while minimizing discomfort, and periodic evaluations allow clinicians to monitor progress and modify the plan as needed. Most patients notice symptom improvement after 2–3 sessions.
Sensations During Treatment and Comfort Measures
Patients may feel a mild tapping, tingling, or warmth at the treatment site as shockwaves penetrate the tissue. Discomfort is usually transient and well-tolerated without anesthesia. Clinicians can adjust energy levels or use cushioning to enhance comfort. Some patients describe a subtle ache that resolves within hours post-session. The procedure’s non-invasive nature ensures minimal disruption, allowing individuals to maintain daily activities immediately. Proper communication between patient and clinician is essential to manage expectations and ensure a comfortable treatment experience.
Recovery Timeline and Post-Treatment Care Recommendations
Recovery following ESWT is minimal, with most patients resuming normal activities immediately. Mild swelling or tenderness may occur for 24–48 hours and can be managed with ice, rest, or elevation. Patients are encouraged to wear supportive footwear and avoid high-impact activities for the first day. Follow-up appointments allow monitoring of symptom progression and determination of additional sessions if necessary. Consistent adherence to post-treatment recommendations, including biomechanical adjustments and footwear optimization, enhances long-term outcomes and reduces recurrence risk, maximizing the therapeutic benefits of shockwave therapy.
Часто задаваемые вопросы (FAQ)
ESWT stimulates tissue regeneration and nerve repair, targeting the underlying neuroma rather than only masking symptoms, providing long-term relief.
Most patients resume normal walking immediately. Mild soreness or tingling may occur for 24–48 hours but resolves quickly without downtime.
For many patients, ESWT is a non-invasive alternative to surgery, particularly when neuroma is moderate or when patients want to avoid surgical risks.
Pain relief often lasts several months to a year. Maintenance sessions may be recommended for persistent symptoms or ongoing biomechanical stress.
ESWT is generally safe; minor swelling or redness may occur. Contraindications include pregnancy, active infections, or certain vascular or nerve disorders.
Unlike injections or surgery, ESWT produces mild tapping, pressure, or warmth sensations. No anesthesia is needed, and the experience is generally comfortable.
Заключение
Shockwave therapy offers a safe, non-invasive solution for Morton’s neuroma, providing an effective alternative to injections or surgery. Focused acoustic waves stimulate tissue regeneration, reduce inflammation, and promote nerve healing, addressing the root cause of neuropathic foot pain rather than masking symptoms. Clinical studies and podiatric experience show significant pain reduction, improved mobility, and enhanced quality of life with minimal downtime. Patients experience rapid relief, long-lasting results, and can return to daily activities quickly. Early treatment and adherence to protocols optimize outcomes and lower recurrence. As podiatrists adopt ESWT in standard care, it is emerging as a preferred, evidence-based approach, delivering durable relief while avoiding risks associated with invasive procedures.
